The use of MRI for knee disorders can improve diagnostic confidence, and it frequently changes clinical diagnosis and patient care management, according to a study presented at RSNA 2011 by researchers from the Cleveland Clinic.
By knowing ahead of time the best course of action to take for knee ailments, based on MRI results, healthcare costs may be reduced, patients may benefit from more effective treatment, and the diagnostic confidence of physicians who may not be skilled in interpreting MRI results may improve.
While MRI is increasingly being used in diagnosing knee pathology, the modality's value in terms of diagnosis and patient care management has been seen as inconsistent in previous studies, noted lead study author Dr. Naveen Subhas, assistant professor of radiology at the Cleveland Clinic.
During his RSNA presentation, Subhas cited previous research that found that preoperative knee MRI can reduce the number of surgeries and uncover a significant number of unsuspected diagnoses, improving the diagnostic confidence for meniscal and anterior cruciate ligaments.
Other past studies, however, concluded that preoperative MRI does not necessarily reduce the number of surgeries performed or affect patient outcomes. MRI also may not significantly change diagnosis or alter the management of patients being considered for orthopedic referral, Subhas added.
Therefore, the purpose of the Cleveland Clinic's prospective study was to determine how frequently knee MRI changes clinical diagnosis and patient management. The group also wanted to determine if such changes relate to specific patient or ordering physician characteristics, and how knee MRI affects diagnostic confidence.
Subhas and colleagues sent questionnaires to three orthopedic surgeons and three sports medicine physicians from the same multispecialty practice, asking them to complete surveys on patients who were scheduled to receive knee MRI scans between June 2010 and January 2011.
They were asked to fill out a pre-MRI survey about each patient's symptoms, physical exam findings, why the MRI was ordered, the anticipated diagnosis, and the planned management of each patient's care.
The survey also asked if surgeons and physicians were planning to correct the condition surgically or nonsurgically. In addition, the sports medicine physicians were asked if the patient needed referral to an orthopedic surgeon.
The study included 93 patients (48 females and 45 males) who had a mean age of 43 years, ranging from 14 to 82 years. Orthopedic surgeons evaluated 54 patients, while sports medicine physicians evaluated the other 39 patients. Each physician completed between 10 and 25 surveys.
Causes for the knee ailments included 44 cases from trauma and injury and 37 cases where there was no trauma or obvious injury. The cause of the knee problem was unknown or missing in 12 cases.
The duration of the knee problem was less than one month for 30 patients, between one and six months in 30 cases, and longer than six months for 32 patients. There was one case in which the time of the ailment was unknown or the data were missing.
Patients proceeded to their MRI scan, after which time the six physicians were polled again and asked the same questions. One key question was if and how the diagnosis and patient care management plan changed following the MRI results.
When the results were tallied, the researchers found that MR images changed the primary diagnosis in 37% of the knee cases (34 of 93 patients) and altered patient care management in 29% of cases (27 of 93 patients).
Frequency of change vs. pre-MRI diagnoses
|
In addition, MRI changed patient management plans in 18 of 52 cases (35%) in which nonsurgical treatment was planned, with 13 of 18 cases headed to surgery. MRI also eliminated surgery in four of 22 cases (19%), and changed the type of surgery in five of 24 cases (21%).
Frequency of change vs. planned management
|
There were some areas in which MRI changed the primary diagnosis significantly.
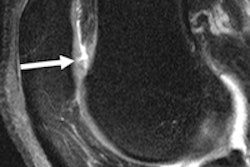
"For example, if the clinician was worried about a lateral meniscal tear or [patients] were having lateral side knee pain, most of the time when they thought there was a lateral meniscal tear, there was no sign [of a tear] on the MRI," Subhas told AuntMinnie.com.
Diagnostic confidence levels in the primary diagnosis after MRI increased 9% when the diagnosis did not change.
"In those cases where diagnosis changed, the confidence in the new diagnosis increased by 15%, but the confidence in their initial diagnosis decreased by about 60%," Subhas added. "Clearly, the MRI altered their thinking of what was going on."
The researchers also found that among patients who were referred to an orthopedic surgeon for surgery, 12% did not need surgery after the MRI results were evaluated.
The study indicates the value of MRI for physicians who are used to dealing with the modality, Subhas said; the results could be even more profound for doctors who are less familiar with the technology.
"What is interesting is that these are studies that were ordered by orthopedic surgeons and sports medicine physicians who are the most skilled in evaluating them," Subhas said. "So, our hypothesis is that often MRI scans are ordered by nonsurgeons, such as family physicians, and in those cases, it will probably affect them even more in terms of changing their diagnosis or management because they are not as familiar with the processes as the subspecialists are."
Subhas and colleagues noted several limitations of their study, including its small sample size of 93 cases and the small number of six participating physicians. Additionally, there was a lack of clinical follow-up to ensure the accuracy of the MRI diagnosis.
"It is a small study, but the purpose is to use [these results] to do a bigger study with funding," Subhas added. "I think this is how we will help control healthcare costs in the future, by doing these kinds of studies and figuring out how often an imaging study like this makes a difference and in what specific circumstances [an imaging study] doesn't make a difference."


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











