The addition of two MRI sequences to a common MR angiography technique can significantly improve the detection of pulmonary embolism (PE), according to a study published online March 19 in Radiology.
Researchers from the University of Arizona College of Medicine achieved a sensitivity of 84% in detecting pulmonary embolism by combining 3D MR pulmonary angiography, low-flip angle 3D gradient-echo, and respiratory-triggered true fast imaging with steady-state precession (FISP) MR sequences. The study was led by Dr. Bobby Kalb from the college's department of radiology.
CT angiography is the gold standard for diagnosis, but it does expose patients to ionizing radiation and iodinated contrast, which carries a risk of allergic reactions and kidney damage in some patients. MRI has been the alternative in detecting pulmonary embolism in pregnant women and patients whose kidneys may be harmed by CT angiography contrast agents.
However, as the authors noted, the Prospective Investigation of Pulmonary Embolism Diagnosis III (PIOPED III) multicenter trial found that centers had difficulty obtaining adequate quality MR pulmonary angiography for suspected pulmonary embolism. The PIOPED researchers determined that MR pulmonary angiography should be considered only at centers that routinely perform the technique well, and for patients who have contraindications to standard tests.
In the current study, the researchers enrolled 22 patients, with an average age of 61 years, who tested positive for pulmonary embolisms on a 64-slice CT scanner (LightSpeed VCT, GE Healthcare) from August 2007 to July 2009. The participants also received a 1.5-tesla MRI exam (Magnetom Avanto, Siemens Healthcare) within 48 hours of the CT scan. The average time between CT pulmonary angiography and MR imaging was 30.3 hours.
Two radiologists with experience in vascular MRI interpreted all the exams. CT pulmonary angiography results were analyzed by a chest radiologist.
In the follow-up analysis, MR pulmonary angiography achieved sensitivity of 55% for pulmonary embolism detection, compared with 67% sensitivity for triggered true FISP and 73% sensitivity for gradient-echo MRI. The combination of all three MR sequences improved overall sensitivity to 84%.
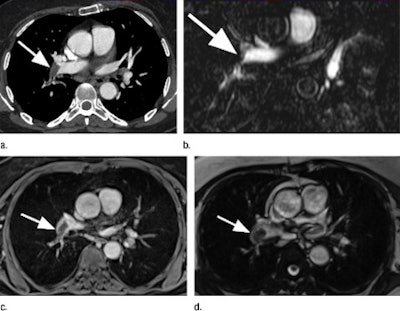 |
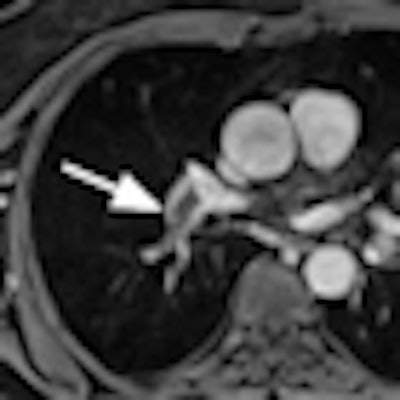
| Pulmonary embolus (arrow) of the right pulmonary artery in a 67-year-old woman. The images include a CT pulmonary angiogram (a), axial reformation of bolus-triggered 3D MR pulmonary angiogram (b), 3D gradient-echo MR image (c), and a triggered true FISP MR image (d). Images courtesy of Radiology. |
CT angiography detected a total of 67 pulmonary emboli, while 56 emboli were detected through the overall MRI exams. The 3D gradient-echo MRI sequence had the highest accuracy, at 90% in diagnosis, while the 3D MR pulmonary angiography sequence showed the lowest sensitivity, at 55%.
The 3D MR pulmonary angiography sequence also produced the only false-positive result for thrombus, although this sequence demonstrated specificity of 99%. No false-positive results were identified among the 3D gradient-echo or triggered true FISP images.
Of the 11 pulmonary emboli not discovered through the MRI techniques, eight emboli were in a segmental pulmonary arterial branch and three emboli were missed in a subsegmental branch.
The findings "lay the foundation for future clinical studies and technical development," Kalb and colleagues concluded.
3D gradient-echo and nonenhanced true FISP sequences with cardiac and respiratory triggering provided "sensitive imaging for the detection of pulmonary embolisms compared with standard bolus-timed MR pulmonary angiography," according to the group. "The combination of all three MR imaging techniques further improved detection of PE, providing a potential diagnostic alternative to CT without the associated risks of exposure to ionizing radiation and iodinated contrast material."




















