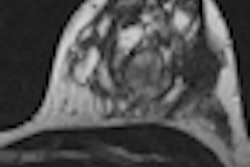
In a large prospective, multicenter trial, researchers found that the recently adopted BI-RADS categories for breast MRI work well in predicting which patients are most likely to have malignant lesions. Mass shape and contrast enhancement patterns were most predictive of cancerous lesions, according to a study published online May 15 in Radiology.
The researchers concluded that the evaluation of lesion features as detected by breast MRI, along with BI-RADS criteria, "enables differentiation of most benign and malignant lesions." The study was led by Dr. Mary Mahoney from the department of radiology at the University of Cincinnati Medical Center.
BI-RADS expansion
The BI-RADS system of classifying suspicious lesions based on their likelihood of malignancy has worked well for years in conventional mammography. Recently, the BI-RADS system was expanded to include both breast ultrasound and breast MRI.
The breast MRI version of BI-RADS includes terms that can be used to describe the unique morphological and kinetic patterns found on breast MRI studies, Mahoney's group wrote. The researchers launched the current study to assess the positive predictive value of BI-RADS for breast MRI, and to identify the lesion features that are most predictive of cancer.
A total of 25 sites and 50 readers were involved in the study to evaluate MRI results from 969 women. The patients underwent breast MRI after negative findings with mammography and clinical exam of the contralateral breast within 90 days of a new diagnosis of breast cancer.
The researchers excluded women who had undergone breast MRI within 12 months before enrollment, were pregnant, or had a contraindication to MRI, such as an implanted magnetic device or severe claustrophobia. Other potential subjects were excluded if a breast cancer diagnosis was made more than 60 days before enrollment or if they had chemotherapy or hormonal therapy for breast cancer within six months before enrollment.
Of the 969 patients, 691 (71%) were assessed in BI-RADS category 1 or 2, with no further evaluation recommended by the radiologist. However, the researchers collected one-year follow-up data for all patients as part of the study protocol. Two BI-RADS category 1 patients had malignancies, as discovered by biopsy, within one year. There were no malignancies among BI-RADS category 2 subjects.
Results according to BI-RADS category
|
|||||||||||||||||||||||||
| Source: Radiology, Dr. Mary Mahoney et al |
There were 106 participants (11%) in the BI-RADS category 3 assessment, with short-term follow-up MRI recommended. Of those patients, 101 (95%) underwent either biopsy or additional evaluation and follow-up. A total of 71 (67%) received follow-up MRI less than eight months after their initial MRI. Of the remaining 35 patients, 13 underwent mastectomy or biopsy, and 17 received either mammography, ultrasound, or MRI more than eight months after the initial MRI scan. Five patients were lost to follow-up.
There were 97 participants (10%) in BI-RADS category 4 or 5. Eighty-three women in BI-RADS category 4 were biopsied, with 17 malignancies diagnosed for a positive predictive value of 21%. Of the remaining 11 patients, seven received targeted ultrasound, two had annual mammography, and one each received short-term follow-up MRI or ultrasound. All results were negative.
All BI-RADS category 5 women were biopsied, with malignancy found in 10 of the 14 patients, resulting in a positive predictive value of 71%.
Mahoney and colleagues also found that lesion shape was a factor in malignancy. An irregular lesion shape had the greatest positive predictive value for cancer at 30%, while an oval-shaped abnormality had the lowest positive predictive value for cancer at just 5%.
As for mass margins, irregular margins at 20% and spiculated or jagged-edged margins at 33% had the highest positive predictive values for cancer. The lowest positive predictive values were found among smooth margins, at 5% positive predictive value.
In addition, masses with significant internal enhancement were most likely to be predictive of cancer, with a positive predictive value of 23%, compared with masses with minimal or moderate internal enhancement. Nonmasslike enhancement was most likely to be malignant in cases of ductal enhancement, with a positive predictive value of 50%.
Interestingly, Mahoney and colleagues noted there were no cases of symmetric nonmasslike enhancements that were cancerous.
The results for positive predictive value were similar to mammography and ultrasound among BI-RADS category 5 lesions, which were "significantly higher than that of BI-RADS category 4 lesions, but lower than the BI-RADS category 5 definition of 0.95 assessed probability of malignancy," according to the group.
"The BI-RADS assessment categories for MR imaging work well to predict the risk of malignancy," the authors concluded. "The risk of malignancy for BI-RADS category 3 lesions is well under 2%."
While BI-RADS category 4 and 5 lesions are at high-risk levels and warrant biopsy, Mahoney and colleagues encouraged the use of the BI-RADS criteria and assessment categories in breast MR imaging.