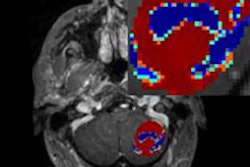
Diffusion-weighted MR imaging (DWI-MRI) can improve diagnostic performance and be a useful adjunct to conventional MRI in detecting prostate cancer, according to a meta-analysis published in the October issue of the American Journal of Roentgenology.
High-resolution T2-weighted MRI traditionally has provided high tissue contrast resolution and helps in cancer staging and assessing the extent of prostate cancer. However, T2-weighted MRI can fall short in distinguishing between a tumor and benign disease, such as inflammatory tissue, wrote lead author Dr. Cher Heng Tan, from MD Anderson Cancer Center's department of diagnostic radiology, and colleagues.
"This shortcoming has led to substantial interest in MRI techniques -- such as diffusion-weighted imaging (DWI), MR spectroscopy (MRS), and dynamic contrast-enhanced MRI (DCE-MRI) -- that can be performed concurrently with anatomic imaging (primarily T2-weighted imaging) by MRI to improve detection of tumor foci in the local assessment of prostate cancer," they wrote (AJR, October 2012, Vol. 199:4, pp.822-829).
DWI's benefits
DWI, in particular, could prove beneficial to patients due to its short acquisition time, no need for contrast, and low technical demand for image postprocessing, the authors wrote.
Tan and colleagues conducted a review of literature prior to December 2010; they found 19 studies with a total of 5,892 lesions that met their criteria. The studies each reported one or more MRI sequences designed to determine if prostate lesions are benign or malignant based on imaging results.
The researchers collected data on factors such as the number of patients in each study, the number of lesions, and total lesions that were positive for prostate cancer. They also tabulated the number of true-positive, false-positive, true-negative, and false-negative lesions for each imaging technique in all 19 studies.
In a comparison between DWI and T2-weighted MRI and combined DWI and T2-weighted MRI, the overall sensitivity and specificity of DWI alone and DWI with T2-weighted MRI outperformed T2-weighted MRI alone. The sensitivity of DWI ranged from 67% to 72%, compared with sensitivity of 57% to 62% for T2-weighted MRI. DWI with T2-weighted MRI had a sensitivity of 69% to 72%.
Specificity for T2-weighted MRI was 74% to 78%, compared with 87% to 90% for DWI and 80% to 85% for combined DWI and T2-weighted imaging.
Regarding contrast-enhanced MRI, its overall sensitivity of 53% to 62% was not significantly different from that of T2-weighted MRI, although contrast-enhanced MRI's specificity was 80% to 85%. Contrast-enhanced MRI was less sensitive than DWI alone or DWI combined with T2-weighted MRI, and it was less specific than DWI alone. Contrast-enhanced MRI's specificity did not significantly differ from that of combined DWI and T2-weighted imaging.
DWI clinical use
The meta-analysis revealed several important findings relative to the clinical use of DWI for detecting prostate cancer, according to Tan and colleagues.
For example, the results support previous research suggesting that DWI's performance alone is superior to that of T2-weighted MRI alone.
In addition, "at a defined specificity of greater than 80% ... combined DWI and T2-weighted imaging is superior to T2-weighted imaging alone and [contrast-enhanced] MRI alone but is similar to DWI alone," Tan and colleagues wrote. "These findings suggest that to achieve high specificity, DWI should be added as an adjunct to T2-weighted imaging."
Because DWI alone outperformed contrast-enhanced MRI, the authors also questioned whether adding more MRI techniques, such as contrast-enhanced imaging, to imaging that already includes DWI and T2-weighted imaging enhances diagnostic results.
Tan and colleagues cited several limitations of their research, including the relatively small sample of studies that met their criteria and the lack of data for them to compare certain DWI parameters, such as magnet strength (1.5 versus 3 tesla) and coil type (endorectal or surface phased-array).
Up to nine of the 19 studies were performed using a surface phased-array coil on a 1.5-tesla MRI scanner, while five studies used endorectal coils on 1.5-tesla systems. Five other studies used surface phased-array coils on 3-tesla MRI systems.
The authors also noted that potential clinical uses of DWI, such as enhanced diagnosis of prostate cancer in post-treatment states, could not be evaluated because of limited data.
"The results of a few individual studies suggest that there may be a role for DWI," they added.


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)