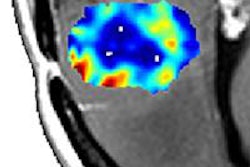
By using dynamic contrast-enhanced MRI (DCE-MRI) and diffusion-weighted MRI (DWI-MRI), physicians can determine if a brain tumor is responding to treatment as soon as two weeks into radiation therapy, according to a study presented on Sunday at the American Association of Physicists in Medicine (AAPM) annual meeting in Indianapolis.
By using the two MRI techniques to measure blood volume and cell density, researchers from the University of Michigan in Ann Arbor were able to see if brain tumors were increasing or decreasing in size in response to treatment that consisted of either whole-brain radiation therapy alone or combined with the tumor-killing drug bortezomib (Velcade, Millennium Pharmaceuticals).
To gauge the success of treatment, patients typically undergo a standard MRI or CT scan after therapy is completed. However, lead author Yue Cao, PhD, a professor of radiation oncology, radiology, and biomedical engineering, said tumors that respond positively to treatment look similar on a CT or MR image for a month or more until the body starts to absorb the tissue.
While physicians wait to confirm the efficacy (or lack thereof) of radiation therapy, patients continue to undergo treatment that may not be working and could miss out on the opportunity to change to a more powerful and more appropriate therapy.
Treatment comparisons
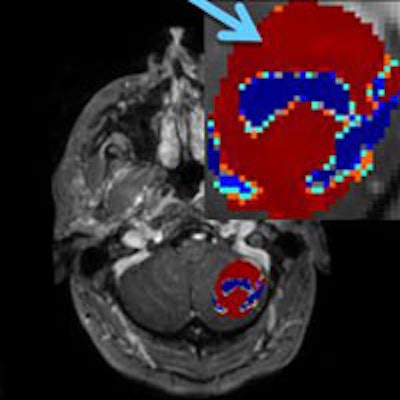
In this study, Cao and colleagues used DCE-MRI and DWI-MRI to image the brains of 24 patients prior to and two weeks after starting radiation therapy to treat a total of 67 brain tumors. All 24 patients also received an MRI exam one month after treatment to confirm tumor size.
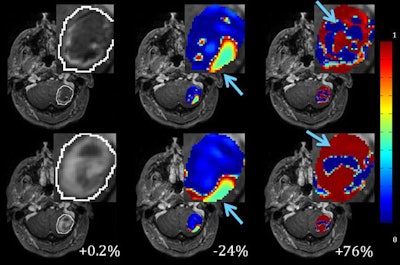
DWI measures apparent diffusion coefficient (ADC) values, which relate to the movement of water molecules in vivo and indirectly reflect tissue microstructural characteristics. The ADC values, in turn, were used to determine tumor volume and categorize them into low, normal, and high ADC results.
Changes in tumor volumes from the start of radiation therapy to the second week of treatment also were evaluated to determine how responsive, stable, or progressive tumors were in patients treated by either whole-brain radiation therapy alone (28 lesions) or whole-brain radiation therapy with bortezomib (39 lesions).
DCE-MRI and DWI-MRI found 24 tumors that had decreased in cell density and/or abnormal blood volume two weeks after radiation therapy, meaning the tumors were responding positively to treatment. The reductions were confirmed by the follow-up MRI results one month into treatment.
Cao and colleagues also found a decrease in both high cellularity and fluid in tissues in lesions that were treated with whole-brain radiation therapy alone, which again confirmed a positive response to treatment. A decrease in the tumor volumes with high cellularity and high vascularity also was confirmed in lesions treated with radiation therapy and bortezomib.
Using receiver operating characteristic (ROC) analysis, Cao and colleagues found that areas under the curve (AUCs) had a value of 0.96 with whole-brain radiation therapy alone and a value of 0.96 with the combination of whole-brain radiation therapy and bortezomib in predicting nonresponsive lesions when changes in different subvolumes were combined.
In addition, gross tumor volume changes could predict nonresponsive lesions treated with whole-brain radiation therapy alone (AUC = 0.91), but could not predict a response in lesions treated with whole-brain radiation therapy combined with bortezomib (AUC = 0.57).
Combining the changes in tumor cellularity and vascularity as visualized on MRI exams "could be used for early prediction of brain metastases response to radiation therapy and [is] better than the gross tumor volume changes, suggesting that physiological changes could occur earlier than the morphological changes," Cao and colleagues concluded.
The importance of the study findings is that MRI with perfusion and diffusion could be used to measure the effect of treatment during therapy, instead of waiting until treatment has been completed, Cao said. If even a portion of a tumor is not responding to treatment, physicians will know sooner and could switch to more appropriate and intensive therapy for the patient.
The research was funded by a grant from the U.S. National Institutes of Health.