By measuring the distance between a tumor and a woman's internal os at MRI before surgical removal of the uterine cervix, or trachelectomy, physicians may be able to identify high-risk patients who should instead undergo a radical hysterectomy, according to a study published in the October Radiology.
Researchers from Memorial Sloan-Kettering Cancer Center (MSKCC) found that a distance of 5 mm or less between the tumor and the internal os (the part of the cervix that opens into the uterus) identifies patients who may need radical hysterectomy.
"Knowledge of this measurement may encourage a surgeon to pursue alternative treatment options, such as neoadjuvant chemotherapy, in the hopes of shrinking the tumor and making fertility-sparing surgery possible," wrote lead author Dr. Yulia Lakhman, from MSKCC's department of radiology, and colleagues (Radiology, October 2013, Vol. 269:1, pp. 149-158).
Conversely, by scanning the area after conization, a form of cervical biopsy, MRI can help confirm that there is no evidence of residual cervical carcinoma and allow patients to avoid unnecessary treatments.
Radical trachelectomy
As the authors noted, radical trachelectomy became an alternative in the late 1980s for young women with early-stage cervical carcinoma who wanted to preserve their fertility. The procedure involves the removal of the uterine cervix, adjacent parametria, and a cuff of the vagina.
At the time, radical trachelectomy was considered only when tumor diameter was less than 2 cm, the distance between the tumor and the internal os was 1 cm or greater, and cervical stromal cancer involvement was less than 50%.
However, some healthcare facilities, including MSKCC, would perform radical trachelectomy if the tumor size was 4 cm or less and other conditions were present. "Therefore, patient selection criteria for radical trachelectomy remain under ongoing investigation," they wrote.
Although preoperative MRI can noninvasively evaluate tumor size and the extent of cancer, Lakhman and colleagues found few studies on the modality's efficacy for determining the most appropriate surgical procedure for these patients.
Patient cohort
The study included 62 patients with a mean age of 32 years (range, 23 to 42 years). All women were diagnosed with stage IB1 cervical carcinoma, had received a preoperative MRI, and had undergone attempted radical trachelectomy between November 2001 and January 2011.
The preoperative MRI was performed to exclude tumor size greater than 4 cm, to make sure the cancer had not reached the parametrium, and to exclude nodal metastases. In all, 32 examinations were done at MSKCC on a 1.5-tesla system (Signa, GE Healthcare). MRI scans performed elsewhere were conducted on MRI scanners of at least 1.5-tesla strength.
Two radiologists interpreted the results and rated tumor presence on a scale of 1, meaning there was no evidence of a tumor, to 5, meaning a tumor was definitively present. The pair also measured tumor size, the distance between the tumor and internal os, and the presence of cancer in the cervix.
All specimens were analyzed by gynecologic pathologists, which served as the standard of reference. The final pathologic analysis showed that 23 (37%) of the 62 patients had no tumors; all tumors had been removed during initial biopsy and/or conization. Of the 39 women with tumors, 15 (38%) had tumors smaller than 10 mm. The largest tumor diameters ranged from 0.1 cm to 3.5 cm, with a mean of 1.47 cm.
Each reader identified nine patients with a tumor-to-internal-os distance of 5 mm or less at MRI, with seven (77%) of nine patients identified by both radiologists. For each reader, radical hysterectomy was required for nine of nine patients (100%) with a distance of 5 mm or less between the tumor and internal os.
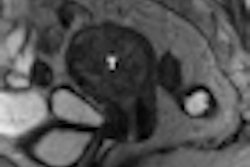
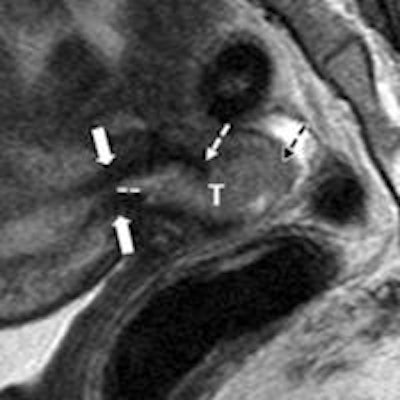
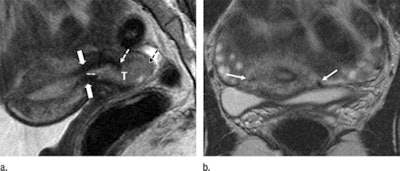 MR images show the tumor-to-internal-os distance and presence of deep cervical stromal invasion in a 23-year-old woman with stage IB1 invasive adenocarcinoma of the uterine cervix. Sagittal (left) and axial (right) images show a tumor (T) within 3 mm of the internal os. Images courtesy of Radiology.
MR images show the tumor-to-internal-os distance and presence of deep cervical stromal invasion in a 23-year-old woman with stage IB1 invasive adenocarcinoma of the uterine cervix. Sagittal (left) and axial (right) images show a tumor (T) within 3 mm of the internal os. Images courtesy of Radiology.For tumors smaller than 20 mm, the mean differences between tumor sizes based on pathology results and MRI were 0.1 mm for the first reader and 1.7 mm for the second reader. For tumors 20 mm or larger, the mean differences were 2.0 mm for the first reader and 3.5 mm for the second reader. Combining their results, eight patients (80%) with tumors 20 mm or larger on MR images received radical hysterectomy.
Regarding deep cervical stromal cancer, MRI found evidence of invasion in 12 (19%) of the 62 patients. Among those 12 women, eight underwent radical hysterectomy.
On a positive note, six women with negative cone biopsy margins and no tumor after conization and MR imaging had no residual carcinoma on trachelectomy pathologic examination.
Treatment strategy
"Our results suggest that tumor distance of 5 mm or less from the internal os at MRI is a statistically significant adverse imaging feature that identifies patients who are likely to require radical hysterectomy," the authors concluded. "Furthermore, MR imaging after a conization with negative margins is useful for confirmation of the absence of tumor in the remaining cervix."
Information received from the MR images "may profoundly affect patient counseling and selection for fertility-sparing treatments," they wrote. "Prospective studies are needed to further assess the value of MR imaging to improve patient selection for fertility-sparing surgery."
Lakhman and colleagues cited several limitations to the study, including its retrospective approach and the small patient cohort that spanned 10 years. In addition, there was a relatively long time between preoperative MRI and surgery for some patients, and only patients scheduled to undergo radical trachelectomy were included in the research, which could have contributed to selection bias.