Sunday, December 1 | 11:45 a.m.-11:55 a.m. | SSA07-07 | Room E450A
Dutch researchers have achieved high accuracy by combining endoscopy, T2-weighted MRI, and diffusion-weighted MRI (DWI-MRI) to assess response to chemoradiation in rectal cancer patients.Based on the results, lead author Dr. Monique Maas, a resident in the department of radiology at Maastricht University Medical Centre, and colleagues now recommend the imaging protocol for restaging rectal cancer when less-invasive treatment is being considered instead of total mesorectal excision.
"Currently, patients with a complete response after chemoradiation for rectal cancer are treated with total mesorectal excision, which is associated with a high rate of postoperative morbidity," Maas told AuntMinne.com. "So far, imaging has had difficulties in safely selecting these complete responders."
Physicians must be able to accurately identify a complete response for less-invasive options, such as local excision, to be considered, according to the researchers.
The study evaluated 49 patients who underwent restaging with T2-weighted MRI, DWI, and endoscopy eight weeks after completing chemoradiation. Of the 49 patients, 18 (37%) had residual tumor and 31 (63%) had a complete response.
The area under the curve (AUC) was 0.71 for T2-weighted MRI, 0.78 for T2-weighted MRI and DWI, and 0.88 for endoscopy. When all three were combined, AUC reached 0.91 for the identification of patients with a complete response.
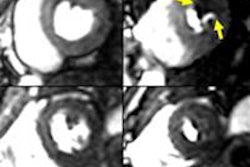
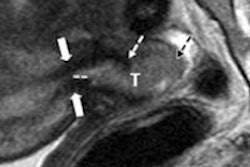
Maas explained that DWI adds information on the response of rectal cancer to chemoradiation, while standard T2-weighted MRI is useful primarily for assessing extramural extent of tumor outside the bowel wall in cases of residual tumor and identification of nodes.
"Endoscopy is of major help to correct for the overestimation of residual tumor that is frequently found when using T2-weighted MRI and also, but less frequently, with diffusion-weighted MRI," she said. "Combining the three imaging strategies thus leads to an accurate selection of complete responders."