Tuesday, December 3 | 3:50 p.m.-4:00 p.m. | SSJ17-06 | Room E451B
A new study by Swiss researchers questions the efficacy of whole-body MRI after the modality falsely classified approximately 25% of healthy subjects as having axial spondyloarthritis.Axial spondyloarthritis is a form of inflammatory arthritis that affects the spine and sacroiliac joints and often causes back pain. A patient with this condition also often has skin psoriasis. The aim of the study was to assess the prevalence of axial skeleton changes by whole-body MRI in skin psoriasis patients without clinical evidence of arthritis.
The study included 25 patients with a median age of 52 years, psoriasis, and no history or clinical evidence of arthritis, along with 25 healthy controls with no history of inflammatory back pain or skin psoriasis.
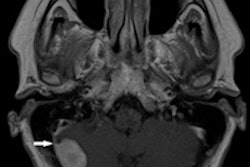
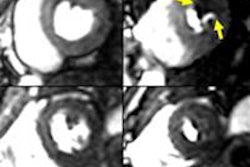
All study participants were examined clinically by the same dermatologist and rheumatologist and underwent noncontrast-enhanced 1.5-tesla whole-body MRI. MR images included both the sacroiliac joints and the entire spine and were read randomly and independently by a radiologist and a rheumatologist.
The analysis of whole-body MR images found that 24% of healthy controls and 30% of skin psoriasis patients were classified as having spondyloarthritis.
Readers achieved a high diagnostic confidence level in 12% of controls and in 18% of patients. There were no statistically significant differences between the two groups regarding assessment of the spine and the sacroiliac joints.
"Based on our pilot study, whole-body MRI doesn't seem to be an appropriate tool to identify those psoriasis patients that will develop spondyloarthritis before clinical disease manifestation," said lead author Dr. Vlad Bratu from the department of radiology and nuclear medicine at University Hospital Basel.
"If these results are confirmed, then it would prevent unnecessary MRI investigations in these patients in an empirical attempt to refer them for spondyloarthritistherapy as early as possible," he added.
Axial inflammation in skin psoriasis patients might be overestimated on whole-body MRI, since matched healthy subjects showed a similar frequency of MRI findings, Bratu and colleagues concluded.