CHICAGO - The complexity and extent of follow-up imaging often required in cases of facial transplantation means the application of all available low-dose imaging techniques must be pursued, according to top award-winning research presented at RSNA 2013.
"Continued evaluation for optimal vascular imaging to determine regional graft perfusion while minimizing overlapping artifact should be considered, comparing traditional and rotational digital subtraction angiography versus developing technologies such as dual CT with iodine mapping," noted Dr. Adnaan Moin and colleagues from the University of Maryland Medical Center, who received a prestigious magna cum laude award on Wednesday for their electronic primer about the use of imaging in facial transplantation.
The authors think there could be a post-transplantation role for bone scintigraphy to verify allograft bone viability, possibly in conjunction with vascular imaging. Given that extensive repairs often are necessary prior to evaluation for a facial transplant, no current role exists for MRI, but in instances of potential acute, primary facial transplantation, MRI and MR angiography may be considered.
"The full imaging armamentarium is required to comprehensively plan full facial composite allotransplantation and care for the recipient in the perioperative period," stated Moin and colleagues.
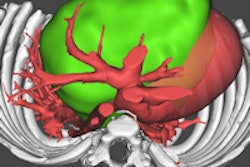
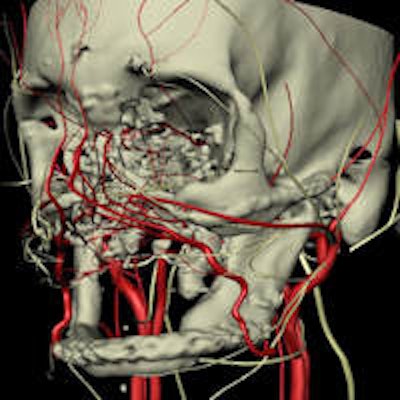
CT with 3D reconstructions is essential to delineate the skeletal anatomy of both recipient and donor. CT angiography provides a global anatomic perspective of the vasculature of recipient and donor, but images can be compromised by surgical clips and hardware, and it does not provide a dynamic assessment of collateral flow. Though invasive, digital subtraction angiography is not as hindered by metal-related artifact, and it provides a dynamic assessment that more clearly defines collateral flow and alterations in arterial flow, they explained.
Since the first partial facial transplant was performed in France in 2005, allogenic facial transplants have continued to evolve, culminating in an extensive facial transplant carried out at the R. Adams Cowley Shock Trauma Center in 2012.
"Clinically, patient selection is reserved for the most severe of facial injuries, such as high-energy central facial trauma with profound tissue loss, where multiple extensive reconstructive procedures have failed in aesthetic and functional restoration," the authors wrote.
For complex post-traumatic facial deformities in patients for whom conventional surgical techniques have rendered functionally and cosmetically unsatisfactory results, imaging plays an essential role in both pre- and postoperative evaluation, they concluded.
In the Lakeside Learning Center in McCormick Place on Wednesday, the authors of 29 education exhibits were awarded a magna cum laude. The highest accolade, summa cum laude, was not presented at this year's meeting.
Editor's Note: The image on our home page was provided by Dr. Darren Smith and Dr. Vijay Gorantla, PhD, from the University of Pittsburgh Medical Center. To prepare for facial transplantation, they create plastic or plaster models based on 3D CT or angiographic images or reconstruction. Following this, mock cadaveric dissections are performed to allow surgeons to plan for the donor and recipient surgeries. By combining information from multiple imaging examinations and creating a sophisticated 3D computer model, they can assess the facial structure and contours; the underlying bone, muscles, nerves, and vessels; and the extent of damage. Smith and Gorantla presented on this topic at RSNA 2011.