You can't manage what you can't measure. This maxim by quality expert W. Edwards Deming can easily be applied to breast MRI: Despite its growing use, the exam still lacks adequate benchmarks for assessing quality, according to a study published in the September Journal of the American College of Radiology.
Researchers from Massachusetts General Hospital (MGH) sought to rectify the situation in one of the largest studies to date on breast MRI in clinical practice. They found a major difference in the performance of breast MRI based on whether it was being used for screening or diagnostic indications (JACR, Vol. 11:9, pp. 883-889).
While many of the results were expected, lead author Dr. Bethany Niell, PhD, an assistant radiologist in the division of breast imaging in MGH's department of radiology, said it's important to keep indications in mind when performing breast MRI audits.
"Breast imagers need to think about whether or not the audit is for screening or diagnostic indications, rather than grouping screening and diagnostic indications together, which could give spurious audit results," she said.
Increased popularity
Annual screening with mammography remains the gold standard for breast cancer screening, but supplemental screening with breast ultrasound or breast MRI has become increasingly popular in recent years.
"There are discrete groups of women in whom supplemental screening with breast MRI, in addition to screening mammography, shows additional cancer detection benefits," Niell said. "Breast MRI has a very high sensitivity for invasive breast cancers, and the sensitivity of breast MRI for ductal carcinoma in situ is also quite high."
 Dr. Bethany Niell, PhD, from Massachusetts General Hospital.
Dr. Bethany Niell, PhD, from Massachusetts General Hospital.A diagnostic breast MRI scan is most commonly used for women with a new diagnosis of breast cancer to evaluate the extent of disease and to detect cancer in the contralateral breast. Screening breast MRI, in addition to screening mammography, is used in high-risk women who have a greater than 20% lifetime risk of breast cancer or who otherwise meet high-risk screening guidelines from the American Cancer Society (ACS).
Dense breast tissue in and of itself is not currently an indication for supplemental screening breast MRI based on ACS and American College of Radiology (ACR) guidelines.
The study was also prompted, in part, by a lack of performance benchmarks for breast MRI in the published literature.
"We performed this study because audit parameters for breast MRI were not defined, available, or published in the BI-RADS Atlas at the time of the study," Niell added.
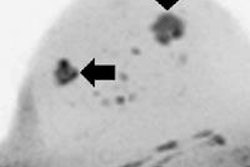
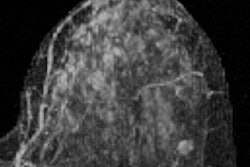
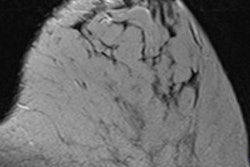
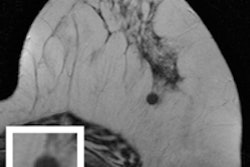
The retrospective study included 2,444 breast MRI examinations performed at MGH between April 1, 2007, and March 31, 2008. The scans were conducted using a 1.5-tesla scanner with a dedicated breast coil. Standard bilateral image acquisition included a multiplanar localizing sequence, along with axial T1-weighted, axial fat-suppressed T2-weighted, and axial and sagittal T1-weighted fat-suppressed sequences performed before and after the injection of 20 mL of gadopentetate dimeglumine (Magnevist, Bayer HealthCare Pharmaceuticals).
"Screening and diagnostic breast MRI almost always include the same imaging acquisition, which makes breast MRI different from mammography or ultrasound," Niell said. "However, because the prevalence of cancer differs in women who are getting screening breast MRI and diagnostic breast MRI, it comes as no surprise that the performance measures differ as well."
Each breast MRI scan was interpreted by one of 10 board-certified radiologists specializing in breast imaging. Studies assigned a BI-RADS category of 0, 4, or 5 were considered to have positive results. Suspicious findings were defined as having a BI-RADS 4 or 5 designation after additional imaging evaluation or workup. A true positive was defined as having a diagnosis of malignancy within one year after a positive result.
Positive predictive values (PPVs) were based on BI-RADS recommendations for mammography. PPV1 denoted a cancer detected after positive results on MRI, PPV2 referred to cancers detected after a biopsy was recommended, and PPV3 denoted cancers detected after a biopsy was performed.
Results
Of the 2,444 breast MRI studies, 1,313 (54%) were conducted for screening, with the most common reasons for the exam being a prior breast cancer (46%) or a family history of breast cancer (26%). The other 1,131 exams (46%) were performed for diagnostic reasons such as problem-solving (37%), short-term follow-up of a breast MRI lesion (33%), or to evaluate the extent of disease in a new breast cancer diagnosis (28%).
The cancer detection rate was significantly lower for screening breast MRI (14 per 1,000 studies) than diagnostic breast MRI (47 per 1,000 studies), the researchers found. In addition, the abnormal interpretation rate for screening MRI was 12% (152 of 1,313), compared with 17% for diagnostic indications (194 of 1,131), a statistically significant difference.
These abnormal interpretation rates are consistent with previous research, according to the authors. For screening, published rates range from 8% to 17%, rising to as much as 22% when screening and diagnostic indications were combined.
A total of 249 lesions were detected by breast MRI and recommended for biopsy. Breast MRI for diagnostic reasons accounted for 172 (69%) of these lesions. Of the 249 biopsied lesions, 79 were malignant, and 61 (77%) of the 79 were from diagnostic exams. The majority of MR-detected malignancies were invasive carcinomas, with no statistically significant difference between screening and diagnostic indications relative to the size of the invasive cancer.
| Breast MRI positive predictive values | |||
| Screening | Diagnostic | Overall | |
| Cancer detected after positive results on MRI (PPV1) | 12% | 28% | 21% |
| Cancer detected after biopsy recommended (PPV2) | 24% | 36% | 32% |
| Cancer detected after biopsy performed (PPV3) | 27% | 38% | 35% |
One key aspect of the study, Niell emphasized, is that the BI-RADS Atlas 5 guidelines had not yet been published at the time of the study. For breast MRI performed at MGH during the study period, BI-RADS category 0 was used for both screening and diagnostic MRI when a radiologist recommended additional imaging evaluation with mammography for a suspicious or indeterminate finding on MRI.
Therefore, the abnormal interpretation rates of 12% and 17% include BI-RADS 0, 4, and 5 results for screening and diagnostic breast MRI. Using more up-to-date criteria with only BI-RADS 4 or 5 exams included after intermodality correlation, the abnormal interpretation rate was 6% for screening and 13% for diagnostic indications, with an overall rate of 9%.
In addition, the authors also considered whether BI-RADS 3 exams would be labeled positive in the most recent BI-RADS Atlas. After correlation with mammography, 277 (21%) screening and 314 (28%) diagnostic breast MRI examinations were assigned final BI-RADS 3 assessments.
Niell highly recommended that radiologists review the new information contained in BI-RADS Atlas 5 regarding audits for breast MRI.
"The recently published audit parameters in BI-RADS Altas 5 now specifically define for breast radiologists how probably benign findings (BI-RADS 3 exams) should be categorized for the audit, based upon screening or diagnostic indication for the exam," she said.
Clinical benefits
The study results are unlikely to change MGH's protocols for the use of breast MRI, Niell noted.
"However, our study results are useful to remind the breast radiologist interpreting a breast MRI that the probability of finding breast cancer would vary based on the indication for the exam," she said. "In other words, a breast radiologist would be more likely to detect a breast cancer on an exam performed for diagnostic indications, rather than screening indications."
Niell and colleagues plan to continue their research regarding breast MRI. One interesting follow-up study would be to investigate whether performance measures differ according to specific screening or diagnostic indications, she said.