
Thanks to a specially modified compact MRI scanner, Cincinnati Children's Hospital Medical Center is having early success in imaging infants in its neonatal intensive care unit (NICU) for pulmonary ailments and abnormal lung development.
A preliminary study by hospital researchers found that free-breathing pulmonary MRI in the NICU with the revamped extremity scanner is feasible and offers diagnostic-quality images for the detection and longitudinal assessment of pulmonary conditions.
 Laura Walkup, PhD, from Cincinnati Children's Hospital.
Laura Walkup, PhD, from Cincinnati Children's Hospital."Our motivation for doing this work is that pulmonary morbidity accounts for a large fraction of our NICU patients," said research fellow Laura Walkup, PhD, during her presentation at the RSNA 2014 meeting. "We don't have a clear picture of the underlying pathologies, and our ability to predict long-term outcomes is lacking. This is, in part, due to poor diagnostics for longitudinal monitoring."
With the modified MRI scanner, "we can see clear pulmonary abnormalities in free-breathing neonates," she added.
A few adjustments
The 1.5-tesla compact MRI is a one-of-a-kind device initially designed for orthopedic use. Cincinnati Children's Hospital modified the scanner for neonatal imaging by raising and leveling the magnet, building a patient table suitable for small infants, and integrating imaging electronics from a high-performance, adult-sized scanner.
As part of an earlier feasibility study, the hospital also used the scanner to perform brain, abdominal, and chest scans on 15 medically stable neonates using standard clinical protocols (American Journal of Roentgenology, January 2014, Vol. 202:1, pp. W95-W105).
The NICU scanner features an 18-cm bore, which can accommodate neonates up to 10 lb. Its gradient coil, which is approximately 2.5 times shorter than the coil in a conventional MRI system, is designed to reduce noise and the chance of peripheral nerve stimulation.
(The scanner was originally developed and marketed by ONI Medical Systems as the MSK Extreme 1.5T for extremity imaging. In November 2009, ONI was acquired by GE Healthcare, which marketed the device as the Optima MR430s for musculoskeletal imaging. GE discontinued the scanner in mid-2014.)
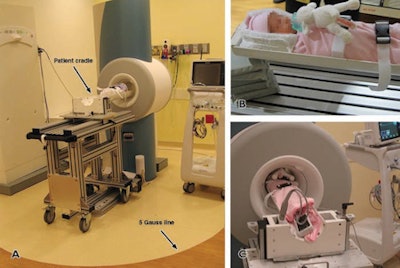 The modified compact MRI scanner (A) sits in the hospital's NICU, while one neonate waits (B) to be imaged and monitored (C). Images courtesy of Laura Walkup, PhD, and the American Journal of Roentgenology.
The modified compact MRI scanner (A) sits in the hospital's NICU, while one neonate waits (B) to be imaged and monitored (C). Images courtesy of Laura Walkup, PhD, and the American Journal of Roentgenology.Neonatal pulmonary imaging poses some inherent challenges because of a neonate's small size, his or her respiratory motion, and the "delicate nature of moving infants to and from the NICU," the researchers noted.
"Although thoracic CT is recognized as the clinical standard, it is inappropriate for neonates," Walkup said. "It's not often ordered, and it's not applicable for longitudinal monitoring. So MRI is an ideal diagnostic modality for these patients in the sense that it is not ionizing and we can image these patients longitudinally."
In their preliminary study, the researchers explored two of the more prevalent pulmonary conditions in the facility's NICU. One was bronchopulmonary dysplasia (BPD), also known as chronic lung disease, which can include interstitial edema, fibrosis, and bronchiectasis. The second condition was congenital diaphragmatic hernia (CDH), an abnormality in the diaphragm that can prevent normal development of the lungs.
Walkup and colleagues imaged a total of 15 NICU patients. This included five full-term control patients with normal lung function, six patients with BPD, and four infants with CDH. All neonates were imaged after repair of their hernia, if necessary, and without sedation.
The MRI protocol included 3D fast gradient-recalled echo (FGRE), fast recovery fast spin-echo (FRFSE), and periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER) techniques.
Walkup estimated that the FGRE and FRFSE scans took about five minutes each, while PROPELLER time was close to eight minutes, bringing the total scan time to approximately 20 minutes.
Image evaluation
The researchers determined that both the FRFSE and FGRE images were generally of diagnostic quality, with very few motion artifacts.
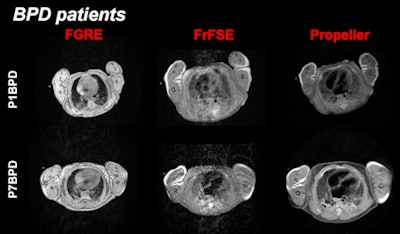 MR images show a more severe case of BPD in the lower row of images (P7BPD). The structural differences are best differentiated in the FGRE sequence and with motion correction by PROPELLER.
MR images show a more severe case of BPD in the lower row of images (P7BPD). The structural differences are best differentiated in the FGRE sequence and with motion correction by PROPELLER.They also noted that pulmonary abnormalities were visually apparent in many cases, with the ability to detect pleural effusion, multiple local areas of atelectasis, alveolar simplification, and parenchymal opacities. MR images of one CDH patient showed regions of trapped air that were undetected in a chest x-ray.
Based on the results, Walkup and colleagues concluded that pulmonary MRI in neonates in the NICU is feasible and can produce diagnostic-quality images without the use of sedation.
"The key here -- not surprisingly -- is that the neonate needs to be quiet," she said. "If the patient is fussy, the images will not look good."
"The technique really speaks to the ability to phenotype and classify by disease severity," Walkup added. "The key point here is that the [MR imaging] techniques are allowing us to longitudinally monitor these patients in ways that were previously inaccessible."




















