
The marathon season is fast approaching, and people training to run those 26.2 miles will endure countless aches, pains, and muscle pulls. Dutch researchers are using diffusion-tensor MRI (DTI-MRI) to gain new insight into the toll that long-distance races take on the human body.
DTI showed changes in the upper legs of athletes after they ran a marathon that were not detected by conventional T2-weighted MRI, the group found.
The additional information gleaned from DTI could be used to personalize rehabilitation and follow-up therapy for injured runners, concluded lead author Martijn Froeling, PhD, from the department of biomedical engineering at Eindhoven University of Technology, and colleagues (Radiology, February 2015, Vol. 274:2, pp. 548-562).
Drawbacks of T2-weighted MRI
Muscle injuries are often diagnosed using T2-weighted MRI with fat suppression, as the imaging technique is effective in detecting abnormalities such as fiber disruption, muscle edema, and hemorrhage. However, previous studies have found that T2-weighted MRI can miss minor tears and muscle fatigue.
"An accurate diagnosis is vital to prevent recurrence of muscle injury," Froeling and colleagues wrote. "Therefore, new methods that are sensitive to subclinical signs of muscle injury are needed to improve diagnosis, which may allow for the design of personalized rehabilitation programs."
Their study evaluated five male amateur long-distance runners with a median age of 51 years (± 3 years), an average height of 6 feet, and an average weight of 190 lb. All five athletes had participated in more than six marathons and trained at least four times per week.
The subjects underwent MRI exams in a 3-tesla scanner (Intera, Philips Healthcare) with a 16-channel receiver coil; they were placed feet first in a supine position. Total imaging time per scan was approximately 45 minutes.
The protocol included T1-weighted MRI for anatomic reference, T2-weighted MRI with fat suppression to assess muscle damage, and DTI-MRI to measure the movement of water molecules in muscle tissue. Images were acquired of the runners' upper legs one week before a marathon, two days after the event, and three weeks after the event. The subjects also received a sports medicine evaluation at each of the three time points.
Froeling and colleagues calculated three DTI-derived values -- tensor eigenvalues, mean diffusivity, and fractional anisotropy -- which are sensitive to changes in tissue microstructure, they wrote.
A radiologist with more than 20 years of experience in evaluating musculoskeletal MRI graded the T2-weighted images with fat suppression by rating muscle injuries on a scale of 0 to 3. A grade of 0 indicated no abnormalities, while a grade of 3 meant complete disruption of the muscle tissue. The reader also noted the location, specific muscle, and craniocaudal and axial length of the edema and/or hemorrhage.
Time-point comparisons
Two days after the marathon, three of the five runners reported stiffness in their hamstring muscles, which resulted in slightly restricted movement, as well as muscle soreness. T2-weighted MRI found nine cases of grade 1 muscle strain among 180 muscles examined.
Also at two days, all three tensor eigenvalues, mean diffusivity, and fractional anisotropy were significantly increased in the biceps femoris (part of the hamstrings), the researchers found. Two of the eigenvalues and mean diffusivity were significantly elevated in the semitendinosus and gracilis muscles (also part of the hamtrings).
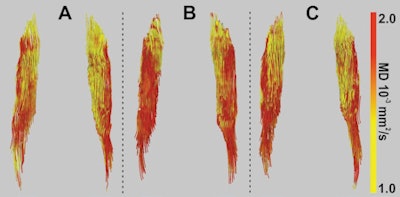 Image shows fiber tractography of the biceps femoris muscle at the three study time points for one marathoner. The fiber tracts are color-coded to show the changes in mean diffusivity. Image courtesy of Radiology.
Image shows fiber tractography of the biceps femoris muscle at the three study time points for one marathoner. The fiber tracts are color-coded to show the changes in mean diffusivity. Image courtesy of Radiology.Tensor eigenvalues and mean diffusivity remained significantly elevated in the biceps femoris muscle three weeks after the run.
Most notably, the muscle changes found by the DTI parameters over time were not detected by T2-weighted MRI with fat suppression.
"Our method revealed subtle changes in DTI-derived parameters of muscle that occurred before the marathon started and after the marathon ended that were still measurable after three weeks," the authors concluded. "These changes were not detected, even in retrospect, with conventional T2-weighted imaging with fat suppression."
Froeling and colleagues cited several limitations of the study, including the small sample size and the lack of a control group. They recommended larger studies before the technique can be applied to clinical practice.




















