In the first study of its kind, researchers from Philadelphia are advocating the use of noncontrast whole-body MRI to screen children who are genetically predisposed to cancer. Their findings were published in the August issue of the American Journal of Roentgenology.
The researchers concluded that 1.5-tesla and 3-tesla whole-body MRI produces "excellent images" and achieves sensitivity and negative predictive value of 100% in this pediatric population. Even though such genetic conditions predisposing children to cancer are relatively rare, these individuals are at significantly greater risk of developing and dying from cancer.
Radiologic screening for malignancies in these children "holds great potential to improve long-term outcomes by maximizing survival and minimizing morbidity from cancers and their treatment," wrote the group led by Dr. Sudha Anupindi from the Children's Hospital of Philadelphia (AJR, August 2015, Vol. 205:2, pp. 400-408).
Screening challenge
Because it is difficult to predict when and where cancer will occur, developing surveillance protocols for these pediatric patients has been a challenge, the authors noted. Whole-body MRI could fill that void because the modality provides "head-to-toe imaging in a single sitting and does not require exposure to ionizing radiation, as with CT or FDG-PET," they wrote.
Anupindi and colleagues retrospectively reviewed 50 MRI scans from 24 children: 18 girls and six boys. The subjects were scanned between 2009 and 2013, and they had a mean age of 11.2 years at the time of the first MRI (range, 2.1-18.2 years). The 50 noncontrast-enhanced whole-body MRI exams were performed on a 1.5-tesla (Avanto or Symphony, Siemens Healthcare) or 3-tesla scanner (Skyra, Verio, or Trio, Siemens) over the five-year period.
The subjects had the following genetic conditions:
- Hereditary paraganglioma-pheochromocytoma syndrome, which is associated with the development of tumors in the paraganglia -- 13 children
- Li-Fraumeni syndrome, which can lead to cancers affecting the breast, brain, soft tissue, blood, and other areas -- 10 children
- Rhabdoid tumor predisposition syndrome, in which patients develop cancer in locations such as the central nervous system and kidneys -- 1 child
The researchers chose those three genetic conditions because they are the most common syndromes for which whole-body MRI is used as part of the children's hospital's surveillance protocol.
Half of the subjects received only one whole-body MRI exam, while the other 12 underwent multiple scans. The average number of examinations per patient was 3.2, ranging from two to eight studies. Because initial scans were performed for screening, no contrast agents were used, although some patients who returned for more regionally specific follow-up MRI scans may have received contrast.
Anupindi and colleagues classified the scan findings according to risk: low (less than 20% chance of malignancy), moderate (20% to 80% chance), or high (greater than 80%). The MRI results were correlated with medical records, biopsy results, or additional follow-up imaging, with biopsy and follow-up used as reference standards.
Overall image quality was found to be "very good" in 48 of the 50 exams; the other two exams were deemed "satisfactory" and still of diagnostic quality, despite patient motion. In addition, the images from 1.5-tesla and 3-tesla MRI scans were comparable, with "very few minor complications associated with sedation, making this modality overall a safe procedure," the authors wrote.
Abnormalities and incidentals
Anupindi and colleagues found abnormalities in nine (18%) of the 50 scans in seven patients. Of the nine abnormalities, two were classified as high risk, two were moderate risk, and five were low risk. One of the high-risk lesions was found to be cancerous at surgery.
Based on the results, whole-body MRI had a sensitivity of 100%, specificity of 94%, positive predictive value of 25%, and negative predictive value of 100%. Coronal and axial short-tau inversion recovery (STIR) sequences were the most effective for detecting abnormalities.
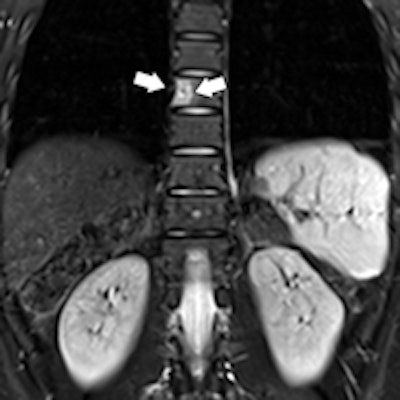
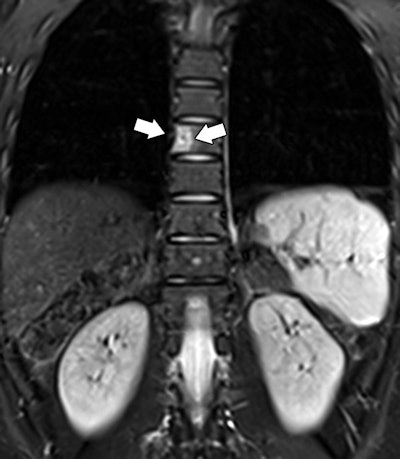 Whole-body MRI of an 18-year-old woman with rhabdoid tumor syndrome. Coronal (above) and axial (below) STIR images show focal hyperintense lesion (arrows) involving T8 vertebral body. The abnormality was considered moderate risk for malignancy and found to be a benign hemangioma on follow-up contrast-enhanced dedicated spine MRI. Images courtesy of AJR.
Whole-body MRI of an 18-year-old woman with rhabdoid tumor syndrome. Coronal (above) and axial (below) STIR images show focal hyperintense lesion (arrows) involving T8 vertebral body. The abnormality was considered moderate risk for malignancy and found to be a benign hemangioma on follow-up contrast-enhanced dedicated spine MRI. Images courtesy of AJR.MRI did also detect 55 incidental findings among 23 of the subjects, the researchers noted.
They stressed that clinicians should inform families of the possibility of incidental findings, but they should also reassure them that "most of these findings do not require further assessment."
"It is important for the radiologist to discuss any findings with the patient's oncologist so that clinical correlation can be made to help stratify the malignancy risk of the abnormality," they added.
Anupindi and colleagues cited several limitations of the study, including its retrospective approach and small cohort. The small size was because cancer-predisposing conditions are rare and there is a lack of research on MRI for this clinical application.
"Despite these limitations, this study is the largest to date to report on clinical experience with whole-body MRI as a cancer screening modality in children," they wrote. "Thus, this study provides important data with a range of clinical implications."