Unfortunately for many who contract COVID-19, neurological effects persist -- and can be tracked on MRI imaging, according to research presented December 4 at the RSNA meeting.
A team led by Yangsean Choi, MD, PhD, of Seoul St. Mary's Hospital in South Korea identified "structural and molecular brain changes specific to cognitively impaired PASC [postacute sequelae of SARS-CoV-2 infection] patients."
Long COVID is typically defined as symptoms that persist beyond four weeks from onset of the illness, and can manifest as fatigue, shortness of breath, and brain fog. But the nature of long-COVID's neurological effects has been mysterious, the group explained.
"Although brain alterations have been reported in PASC infection, the extent to which they are universally present and associated with neurodegenerative processes [has remained] unclear," it wrote.
Choi and colleagues conducted a study that assessed brain MRI results in 209 participants, all of whom had experienced mild COVID at least three months prior to the start of the research. All patients underwent multimodal brain MR imaging. The researchers categorized them into the following three groups:
- Cog-PASC: PASC with cognitive impairment (assessed by Montreal Cognitive Assessment, or MoCA, scores under 26, which indicates mild to moderate impairment).
- Other-PASC: PASC without cognitive impairment but with other symptoms such as fatigue (measured by the Fatigue Assessment Scale, with scores of 22 or higher indicating fatigue).
- NS-PASC: No significant PASC symptoms.
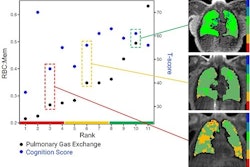
They tracked MRI biomarkers such as cortical thickness and choroid plexus volumes from 3D T1-weighted images, diffusion tensor imaging along the perivascular spaces (DTI-ALPS), and quantitative susceptibility mapping (QSM).
Overall, the team found that Cog-PASC patients were older than those in the NS-PASC and Other-PASC groups (p < 0.001) and had worse cognitive performance (MoCA score 24 for Cog-PASC patients vs. 28 in both other groups; p < 0.001).
It also reported the following:
- MRI showed reduced cingulate cortical thickness in Cog-PASC patients (2.445 mm) compared with NS-PASC (2.449 mm) and Other-PASC patients (2.497 mm).
- QSM showed increased paramagnetic susceptibility, particularly in the cingulate cortex and hippocampus, which is consistent with iron deposition.
- Choroid plexus volume was also higher in Cog-PASC patients compared to Other-PASC patients, correlating with markers of neuronal/astroglial damage and iron accumulation.
- There were no significant differences in DTI-ALPS metrics among the three groups.
The study results provide evidence of "persistent neurodegeneration in a subset of nonhospitalized individuals following mild COVID-19," according to the researchers.
"These findings support a biological basis for cognitive symptoms even after mild COVID," Choi concluded.