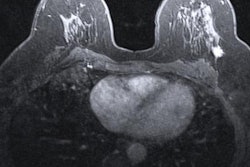
A shortened protocol for breast MRI is just as effective in finding cancer as a full protocol, and it can cut the time a patient is in the magnet by almost 90%, according to a study published online May 11 in Academic Radiology.
The finding is good news for women at high risk of the disease, wrote a team led by Dr. Babita Panigrahi of Johns Hopkins Medicine. Annual screening breast MRI is recommended for these women, but the cost is significant -- which is why researchers have been exploring whether an abbreviated breast MRI protocol is as effective as a full one.
"Breast MRI demonstrates impressive cancer detection rates in high-risk women and is known to be the most sensitive screening tool, but is costly and can be difficult to tolerate due to long scan times," Panigrahi and colleagues wrote."Abbreviated MRI protocols may provide opportunity to minimize time, costs, and patient discomfort."
Short and sweet
Screening breast MRI is a different type of assessment than a diagnostic exam, and the researchers wondered if it's really necessary to use the full protocol for screening, corresponding author Dr. Susan Harvey told AuntMinnie.com.
 Dr. Susan Harvey from Johns Hopkins.
Dr. Susan Harvey from Johns Hopkins."We wondered why we were screening high-risk women with MRI in the same way we were evaluating women already diagnosed," she said. "We suspected that a screening exam wouldn't require the same amount of time in the magnet as a diagnostic exam might."
Panigrahi and colleagues reviewed 1,052 breast MR images acquired using the abbreviated protocol, followed by immediate review of additional images included in a full diagnostic protocol. The group recorded BI-RADS assessments for both and also calculated the cancer detection rate, positive biopsy rate (PPV3), sensitivity, and specificity.
The abbreviated protocol included the localizer series, a precontrast T1-weighted sequence with fat saturation, and one postcontrast T1-weighted sequence with fat saturation, according to the group.
For both protocols, the researchers found a cancer detection rate of 13.3 cancers per 1,000. The PPV3 rate for the full protocol was 30.4%; for the abbreviated sequence, it was 31.1%. Agreement between BI-RADS assessments with the two protocols was 96.6%, and sensitivity and specificity for both did not differ significantly.
| Full vs. abbreviated breast MRI protocol | ||
| Full protocol | Abbreviated protocol | |
| Magnet time | 24 minutes | 3 minutes |
| Cancer detection rate | 13.3 cancers per 1,000 | 13.3 cancers per 1,000 |
| Sensitivity | 81.8% | 81.8% |
| Specificity | 97.4% | 97.2% |
| PPV3 | 30.4% | 31.1% |
The researchers based their clinical decisions on the full breast MRI protocol, given that they were testing the shortened sequence's performance, Harvey said. The full sequence resulted in a change in the final BI-RADS assessment in 3.4% of cases, most of which did not change clinical management in terms of biopsy.
"We found all the cancers using the abbreviated protocol, but given that we didn't have proof that it was comparable -- this was a pilot study -- we did the full sequence for everyone," she said.
How much time did the abbreviated sequence save? Quite a bit: Magnet time for the full protocol is 24 minutes, compared with three minutes for the abbreviated protocol, Harvey said.
"Who wouldn't want to spend 20 minutes less time in the magnet?" she said.
Practice effect?
The American College of Radiology (ACR) has guidelines for breast MRI that a facility must meet in order to be accredited, and it has yet to weigh in on abbreviated sequences, Harvey said. However, the group's own work and that of Dr. Christiane Kuhl of the University of Aachen in Germany, who has also studied shortened breast MRI sequences, has led Johns Hopkins to use a protocol that's somewhere between the full sequence and the abbreviated one. The department takes out a third postcontrast sequence and a delayed postcontrast sequence for an exam that lasts about 13 minutes.
"We have made clinical changes based on this evidence and Dr. Kuhl's research," she said.
Can these results translate to general practice? Panigrahi and colleagues conceded that their study was performed at an academic institution with dedicated breast imagers, and the findings may not be generalizable to practices where general radiologists interpret breast imaging.
"To address concerns regarding the generalizability of this abbreviated technique, we plan to collaborate with several community practice groups to gather similar data in the setting of general radiologists who do not specialize in breast imaging," they wrote. "We believe this additional information will be beneficial for further predicting the scalability of an abbreviated high-risk screening concept."
Harvey also sees changes in technology coming that could shorten breast MRI exams in another way.
"We're in conversation with some MRI vendors who are exploring whether sequences can be shortened, rather than eliminated," she said. "So we could see new technology soon that reduces breast MRI exam time."