Used properly, magnetic resonance enterography (MRE) can play a valuable clinical role in a variety of small-bowel disorders, according to Iranian researchers, who have revealed the 10 main lessons learned from conducting around 1,100 examinations over the past four years.
MRE has become the modality of choice in the diagnosis and follow-up of inflammatory bowel disease (IBD), and can also be used in other cases involving the small bowel, explained Dr. Amir Reza Radmard and colleagues from the department of radiology at the Shariati Hospital, Tehran University of Medical Sciences in Tehran, in an e-poster presentation at RSNA 2017.
At the Shariati Hospital, all 1,100 investigations were performed on a 1.5-tesla scanner (Avanto, Siemens Healthineers), using an 18-channel torso-phased-array coil. Every patient followed a 48-hour low-residue diet and six hours fasting prior to the examination.
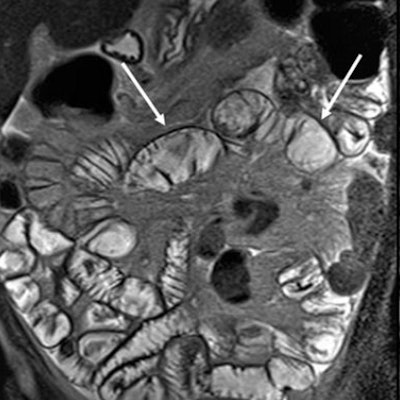
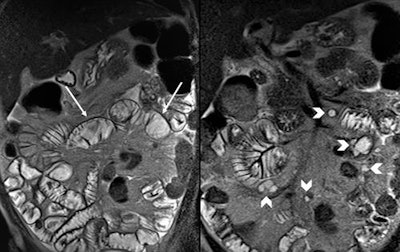 Coronal T2-weighted half-Fourier acquisition single-shot turbo spin-echo images at cavitating mesenteric lymph node syndrome in a case of refractory celiac disease, which display decrease in number of jejunal folds (arrows) along with cystic mesenteric lymph nodes (arrowheads). All images courtesy of Dr. Amir Reza Radmard.
Coronal T2-weighted half-Fourier acquisition single-shot turbo spin-echo images at cavitating mesenteric lymph node syndrome in a case of refractory celiac disease, which display decrease in number of jejunal folds (arrows) along with cystic mesenteric lymph nodes (arrowheads). All images courtesy of Dr. Amir Reza Radmard.A measure of 1,500 mL of polyethylene glycol (PEG) was administered orally at three aliquots (each aliquot: two packets, 25 g, of PEG dissolved in 500 mL of water, consumed in 15 minutes). A single dose of metoclopramide (10 mg) with the first aliquot to promote gastric emptying, and if bowel distension was not satisfactory, an additional 500 mL of water was given over the next 15 minutes. To decrease bowel peristalsis, IV hyoscine N-butyl bromide (20 mg) was administered when the distension of the small bowel was satisfactory on the first sequence (coronal T2-half-Fourier acquisition single-shot turbo spin-echo, HASTE).
The authors highlighted the following key points:
- MRE in amyloidosis may show nonspecific features such as diffuse and uniform thickening of the small bowel wall, dilated loops, increased number of mucosal folds in ileum (jejunization), and loss of normal mural stratification. Relative T2 hypointensity of uniformly thickened bowel wall in comparison with muscle signal might be a useful sign to consider amyloidosis in an appropriate clinical setting.
- In a patient with refractory celiac disease who has experienced recent deterioration of signs and symptoms, the presence of enlarged cystic mesenteric lymph nodes in addition to the typical findings of Celiac disease (fold reversal pattern) can help to make a diagnosis of cavitating mesenteric lymph node syndrome.
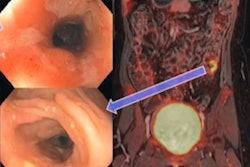
- On MRE, small intestine adenocarcinoma may present as a mass lesion, mainly with intraluminal growth pattern or annular luminal narrowing with overhanging edges. Also, a gastrointestinal stromal tumor (GIST) may present as a well-defined exophytic mass, which is clearly demarcated from the mesentery, and MR signal will be affected by the presence of hemorrhagic, cystic, and necrotic components.
- Diffusion restriction caused by hypercellularity of tumor may raise suspicion for bowel lymphoma, especially in mass-forming type. Adjacent enlarged mesenteric lymph nodes suggest lymphoma rather than adenocarcinoma.
- In patients undergoing diagnostic workup for probable IBD, the presence of any skin lesion should be taken into account, because characteristic skin lesions of Kaposi's sarcoma may help to avoid overdiagnosis of IBD.
- Nontransmural mucosal thickening of distal small bowel along with continuous large bowel involvement and fixed patulous ileocecal valve support the diagnosis of backwash ileitis in cross-sectional imaging.
- Tuberculosis results in mesenteric, porta hepatis and peripancreatic lymphadenopathy with characteristic central caseous necrosis and peripheral rim-like enhancement.
- MRE is unreliable for differentiation between IBD and nodular lymphoid hyperplasia (NLH). Although the findings are less severe compared with those of Crohn's disease, there is considerable overlap. However, lack of dominant involvement of the mesenteric side or mesenteric engorgement may help in differentiating NLH from Crohn's disease.
- Duplication cyst might be overlooked easily on MRE due to its similar signal intensity with intraluminal fluid of bowel especially on T2-weighted sequences. In contrast, a CT scan with positive oral contrast may better delineate it.
- Segmental stricture of the bowel on MRE with adjacent prominent collateral vessels detected in a patient with long-standing hypercoagulability state and findings of chronic mesenteric vein thrombosis should raise suspicion for ischemic strictures.
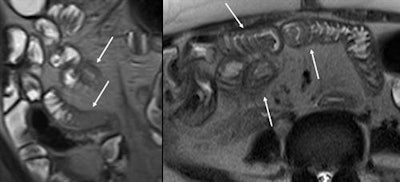 Coronal and axial T2-weighted HASTE images at cytomegalovirus enteritis in HIV positive patient showing mural thickening with T2 hyperintense appearance (arrows).
Coronal and axial T2-weighted HASTE images at cytomegalovirus enteritis in HIV positive patient showing mural thickening with T2 hyperintense appearance (arrows). Dr. Amir Reza Radmard.
Dr. Amir Reza Radmard.