Determining the best course of therapy for stroke patients depends largely on when their stroke symptoms began. But what if they were asleep when their stroke started? Fortunately, a combination of MRI protocols could offer a possible solution, according to a report published April 25 in the Annals of Neurology.
Researchers from Massachusetts General Hospital (MGH) found that a discrepancy between two types of MRI scans performed on "wake-up" stroke patients could be used to estimate the amount of tissue damage and, thus, when the stroke had started. This, in turn, could determine if the patients qualified for tissue plasminogen activator (tPA) therapy (Ann Neurol, April 25, 2018).
"Our study showed -- for the first time -- that tPA could be given safely to patients with stroke of unwitnessed onset, if their imaging suggested the stroke was very early in its progression and they met other treatment criteria," said co-lead author Dr. Lee Schwamm, director of the MGH Comprehensive Stroke Center, in a statement. "These results pave the way for a large randomized trial of tPA in patients with unwitnessed strokes."
Stroke spotting
Currently, the only drug therapy approved by the U.S. Food and Drug Administration (FDA) for ischemic strokes is tPA, the authors noted. Its use is restricted to patients whose stroke was not caused by the rupture of a blood vessel and who are still within 4.5 hours of stroke onset.
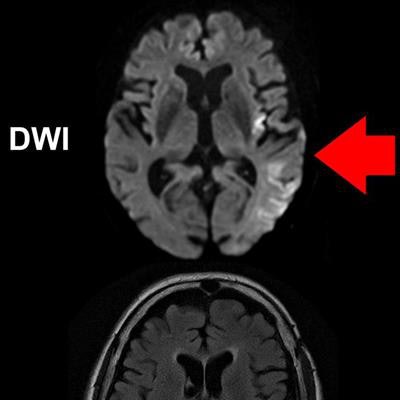
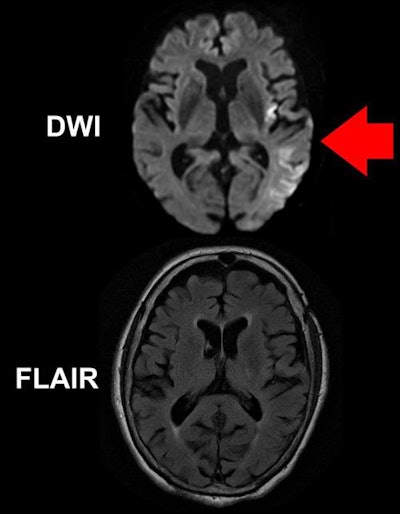 A DWI-MRI scan (top) of a brain shows brighter areas suggesting stroke damage (red arrow). A FLAIR scan (bottom) taken at the same time reveals no obvious acute ischemic damage. Image courtesy of Ona Wu, PhD.
A DWI-MRI scan (top) of a brain shows brighter areas suggesting stroke damage (red arrow). A FLAIR scan (bottom) taken at the same time reveals no obvious acute ischemic damage. Image courtesy of Ona Wu, PhD.The guidelines state that tPA should not be used for wake-up stroke patients (roughly 25% of emergent cases) who did not witness the onset of symptoms because they were sleeping when it occurred. Using tPA can potentially lead to additional harm in patients if the stroke has caused too much damage to brain tissue.
Nevertheless, several clinical studies have reported that giving tPA to these wake-up stroke patients had a positive effect in cases where the patient's MRI scans suggested the ischemic stroke had not yet caused extensive tissue damage.
Building on these findings, Schwamm and colleagues assessed stroke progression in 80 patients at 14 U.S. health centers using two MRI protocols: diffusion-weighted imaging (DWI) and fluid-attenuated inversion recovery (FLAIR). The high sensitivity of DWI makes it suitable for detecting changes in blood flow through the brain in the first minutes after stroke onset, whereas FLAIR generally reveals the effect of stroke on the brain after several hours of reduced blood flow.
In 70% of the wake-up stroke patients, the authors observed early reductions in blood flow to the brain on DWI-MRI scans but no noticeable changes on FLAIR MRI scans -- a difference they referred to as quantitative DWI-FLAIR mismatch (qDFM). This mismatch suggested that these patients were still in the early stages of their stroke, meaning that tPA treatment could be a viable option for them.
"Brain tissue that is abnormal on DWI but not yet abnormal on FLAIR has been seen in patients ... four hours or less after known symptom onset," said co-lead author Ona Wu, PhD. "That discrepancy provides a snapshot of tissue evolution as stroke progresses in the first few hours, and that is the pattern we used to select patients for treatment, since they were likely to be similar to patients with known symptom onset who have benefited from tPA."
Damage-based treatment
By combining the results of DWI and FLAIR, clinicians may be able to increase the number of stroke patients who could safely receive intravenous tPA therapy, which could help reduce stroke-related disability and mortality, according to the authors.
"Rather than treating based on the number of hours since a stroke began, we can treat based on how much damage the stroke has already caused and how much brain can still be saved," Schwamm said.
In the future, the researchers plan to conduct a placebo-controlled trial evaluating the potential benefit of using CT instead of MRI to spot patients with unwitnessed strokes and determine their eligibility for tPA treatment.
"If that phase III study is successful, it would lead to a paradigm shift in the way acute stroke patients are treated," he said. "Because the imaging methods we will use in our phase III study are available on any MRI or CT scanner in use today, if the results of that trial are positive, the approach could be put into practice immediately."