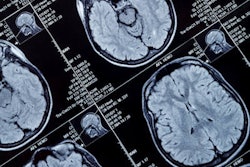
Using MRI, researchers found that lifestyle factors can increase the risk of stroke and dementia later in life among young adults with no clinical evidence of cerebrovascular disease and a seemingly healthy cardiovascular risk profile. The study was published in the August 21 issue of the Journal of the American Medical Association.
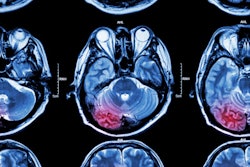
Investigators from the U.K. and Canada found lower density of blood vessels, slower blood flow, and more white-matter hyperintensity lesions on brain MRI scans, which have been linked to the development of stroke and dementia. Assessments pointed to factors such as higher systolic blood pressure, smoking, greater alcohol consumption, and higher body mass index (BMI) as causes.
"We have known for some time that lifestyle during young adult life is relevant to the health of the heart," lead researcher Paul Leeson, PhD, a professor of cardiovascular medicine at the University of Oxford, said in a statement. "This new research is exciting because we have been able to show that similar factors may also be impacting on the health of the brain, decades earlier than previously anticipated."
Early adulthood
The risk of stroke and brain atrophy later in life can be traced back to a person's cardiovascular risk factors in early adulthood. In addition, MR images of cerebral injury in a person's midlife have been associated with future stroke, dementia, and mortality. However, it remains unknown to what degree, if any, cerebrovascular changes are present in young adults based on certain aspects of their lifestyle.
"Young adult cardiovascular health is often a neglected area," added study co-author Dr. Wilby Williamson, a clinical research fellow in cardiovascular medicine at the University of Oxford. "This study is a first step towards personalized risk assessment so we can better inform people about steps to improve their future brain health."
The study included 125 participants between the ages of 18 and 40 years (mean age, 24.7 ± 5 years) with no clinical evidence of cerebrovascular disease. Among the subjects, 29 had a history of hypertension and 21 were taking antihypertension medications (JAMA, August 21, 2018, Vol. 320:7, pp. 665-673).
The subjects underwent a cardiovascular risk assessment, completed a detailed lifestyle questionnaire, and had seven days of measured physical activity. They also received a score based on eight modifiable factors (with one point awarded for each category):
- BMI less than 25
- Highest level of cardiovascular fitness and/or physical activity
- Alcohol consumption of less than eight drinks per week
- No smoking for more than six months
- Blood pressure on awake ambulatory monitoring lower than 130/80 mm Hg
- Nonhypertensive diastolic response to exercise
- Total cholesterol level less than 200 mg/dL
- Fasting glucose level less than 100 mg/dL
MRI scans were performed during a fasting state and before exercise on a 3-tesla system (Magnetom Trio Tim, Siemens Healthineers). The protocol included T1-weighted structural, T2-weighted fluid-attenuated inversion-recovery (FLAIR), diffusion-tensor (DTI), and time-of-flight MR arteriogram (MRA) imaging.
The researchers used the Brain Intensity Abnormality Classification Algorithm (BIANCA) to segment and analyze white-matter hyperintensity lesions and related volumes. In addition, they looked at cerebral blood flow and blood arrival time in a subgroup of 52 participants.
Up in smoke
The subjects had a mean score of 6.0 (± 1.4) for modifiable cardiovascular risk factors at recommended levels, the researchers found.
In correlating the data with MR images, they found that systolic blood pressure (-0.02 vessels/cm3 per mm Hg, p = 0.046), smoking (0.17 vessels/cm3 per pack-year, p = 0.004), and body mass index (-0.08 vessels/cm3 per one BMI unit, p = 0.02) correlated significantly with vessel density. In addition, systolic blood pressure (-0.6 µm per mm Hg, p = 0.03) and smoking (4.0 µm per pack-year, p = 0.04) correlated significantly with vessel caliber.
Smoking (0.8 lesions per pack-year, p = 0.02) correlated significantly with the number of white-matter hyperintensity lesions, along with exercise diastolic blood pressure (0.1 lesion per mm Hg, p = 0.04) and alcohol consumption (0.4 lesions per weekly alcoholic drink, p = 0.03).
Based on previous research, cerebral blood flow is thought to decline with age; older adults are two to three times more likely to develop dementia when cerebral blood flow is below 55 mL/100 g/min. In addition, lower vascular density has been linked to vascular dementia in adults with an early diagnosis of disease.
By comparison, the subset of participants in the lowest tertile for modifiable cardiovascular score had lower vessel density and a mean cerebral blood flow of 55 mL/100 g/min, which placed them in the bottom 40% of the current study population.
"Therefore, the distribution of MRI findings observed in the current study raises the potential that some individuals may be starting to diverge to different risk trajectories for brain vascular health in early adulthood," the authors wrote.
"The observed association between brain vascular measures and modifiable risk factors raises the potential for targeted intervention to prevent progression to disease," they also noted. "Reducing multiple risk factors can change risk trajectories and reduce vascular disease burden."
The findings suggest that regular exercise, sensible drinking, not smoking, and keeping blood pressure at healthy levels can have widespread benefits for both heart and brain disease at any age, the group concluded. The study also "demonstrates the power and utility of medical imaging to better understand how specific risk factors relate to early brain changes," added study co-author and university research lecturer Dr. Adam Lewandowski.
The authors noted that further research is needed to verify the findings and determine their clinical importance. Several of the researchers are also using advanced MRI techniques in a trial with young adults with higher blood pressure. Their goal is to determine ways to change lifestyle to improve brain and heart health.