
Which MRI markers of vascular brain injury are most significantly associated with a greater risk for stroke, dementia, and death in older adults? If you answered white-matter hyperintensities, brain infarcts, and cerebral microbleeds, your conclusion matches the findings of a meta-analysis published online October 22 in JAMA Neurology.
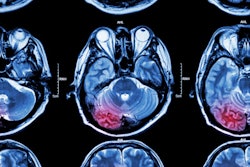
European researchers found that individuals with those three markers had more than twice the risk of ischemic stroke and more than three times the risk of intracerebral hemorrhage. The findings not only advance current knowledge about the risks of vascular brain injury but also could provide the foundation for more effective and tailored ways to treat and prevent common age-related disorders and mortality.
"From a practical perspective, the discovery of these MRI markers should prompt detailed assessment of a person's risk for stroke and dementia and careful evaluation of the benefit-risk ratio for available preventive strategies," wrote lead author Dr. Stéphanie Debette, PhD, from the University of Bordeaux in France, and colleagues.
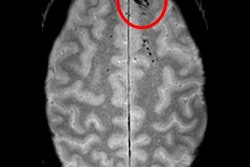
Vascular brain injuries are often detected as incidental findings during routine MRI scans. How those unexpected MR images are "interpreted and acted on presents a common clinical challenge," the authors wrote.
"Individual studies have suggested that MRI markers of covert vascular brain injuries predict an increased risk of stroke, dementia, and death, but other studies did not show any association," they wrote. "Better understanding of the association of specific MRI markers of vascular brain injuries with outcomes is crucial to optimize prevention strategies."
The researchers found a total of 94 prospective, longitudinal studies with more than 16,000 participants in a PubMed search that spanned more than 50 years. Outcome measures were based on stroke, dementia, and death.
The meta-analysis revealed that extensive white-matter hyperintensities on MRI scans were significantly associated with a higher risk for all six adverse outcomes shown in the following table. Brain infarcts showed the same association in five categories, while cerebral microbleeds had four categories. In particular, the presence of all three markers indicated that the individual had double the risk of stroke and more than triple the risk for an intracerebral hemorrhage, as measured by hazard ratios.
| Association of MRI markers with increased risk of adverse outcomes | ||||||
| MRI marker | Stroke | Ischemic stroke | Intracerebral hemorrhage | Dementia | Alzheimer's disease | Death |
| White-matter hyperintensities | ||||||
| Hazard ratio | 2.45 | 2.39 | 3.17 | 1.84 | 1.50 | 2.00 |
| p-value* | < 0.001 | < 0.001 | 0.002 | < 0.001 | < 0.001 | < 0.001 |
| Brain infarcts | ||||||
| Hazard ratio | 2.38 | 2.18 | 3.81 | 1.29 | 1.06 | 1.64 |
| p-value* | < 0.001 | < 0.001 | < 0.001 | 0.04 | 0.64 | < 0.001 |
| Cerebral microbleeds | ||||||
| Hazard ratio | 1.98 | 1.92 | 3.82 | 1.41 | 1.18 | 1.53 |
| p-value* | < 0.001 | < 0.001 | < 0.001 | 0.13 | 0.49 | < 0.001 |
A lack of studies on perivascular spaces prevented a reliable conclusion for that MRI marker, but the available data suggested that high perivascular space burden was associated with an increased risk of stroke, dementia, and death.
"This research highlights the urgent need for randomized clinical trials to assess the benefit-risk ratio of prevention strategies for individuals carrying these markers, such as aspirin and intensive blood pressure-lowering treatment," Debette and colleagues wrote.


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











