Is 7-tesla MRI ready to stake its claim in the radiology department? Currently, three institutions in the U.S. have begun using 7-tesla magnets for clinical applications, but mostly for neurological and musculoskeletal conditions. The challenge now is showing how much more 7-tesla MRI can contribute to patient care.
The Mayo Clinic in Rochester, MN, was the first institution in October 2017 to begin clinical use with 7-tesla MRI, followed by Brigham and Women's Hospital (BWH) in Boston this past September and the University of Southern California (USC) in November.
Needless to say, there is more to 7-tesla MRI than simply plugging the machine into an electrical socket and wheeling in the first patient.
"One of the things we had to instruct people on is that [7 tesla] is not just a 'suped-up' 3-tesla scanner on steroids," said Dr. Kirk Welker, an associate professor of radiology at the Mayo Clinic. "There are some applications that the 7-tesla scanner does exceptionally well that cannot be done on any other clinical scanner. On the other hand, there are applications that are challenging to do on a 7-tesla scanner ... [and] there are the limitations."
A whole new world
 Dr. Kirk Welker from the Mayo Clinic.
Dr. Kirk Welker from the Mayo Clinic.All three facilities are using Siemens Healthineers' Magnetom Terra 7T MRI scanner, which has 510(k) clearance from the U.S. Food and Drug Administration (FDA) for clinical imaging of the brain and knee. Currently, 7-tesla MRI is restricted to those two applications because only a head and knee coil have been cleared by the FDA for use with the ultrahigh-field scanner.
Other vendors manufacture coils to image other body parts on the Terra, but those accessories have not yet been cleared for clinical use, according to Siemens. Thus, 7-tesla imaging performed elsewhere on the body is considered investigational.
Since the installation of the 7-tesla MRI scanner at Brigham and Women's Hospital, clinicians have pursued a "stepwise progression toward nominal operation, where we would initially focus on a couple of indications where 7 tesla demonstrated great value in the research realm," said Dr. Srinivasan Mukundan, PhD, medical director at BWH. "Those two areas are epilepsy and multiple sclerosis."
So how does 7-tesla MRI contribute to the diagnosis of patients with these conditions?
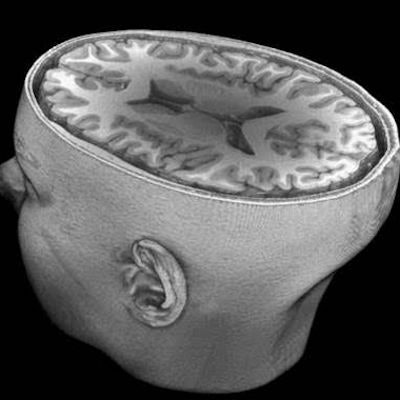
"The simplest answer is that we have better signal-to-noise ratios at 7 tesla that basically translate into higher-resolution images," Mukundan explained. "That allows us to resolve issues that are not easily seen at the lower field strengths. Tiny structural anomalies that are not well-discernible at lower field strengths, for example, in epilepsy and multiple sclerosis, have the advantage of 7 tesla."
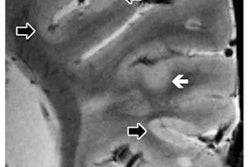
More specifically, with 7-tesla MRI, BWH clinicians can see minute central veins within white-matter plaques of the brain's parenchyma. Gray-matter and cortical lesions are also identifiable at 7 tesla to evaluate these two conditions, he added.
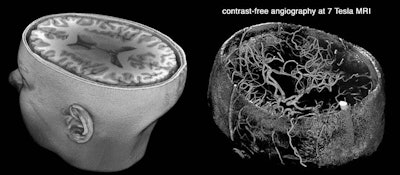 A 3D rendering of a 7-tesla brain MRI scan (left). Time-of-flight MR angiography (right) images blood flow without the need to administer contrast. One of the main applications of 7-tesla MRI is in the diagnosis of intracranial aneurysms. Image courtesy of Dr. Farshid Sepehrband and Arthur Toga, PhD.
A 3D rendering of a 7-tesla brain MRI scan (left). Time-of-flight MR angiography (right) images blood flow without the need to administer contrast. One of the main applications of 7-tesla MRI is in the diagnosis of intracranial aneurysms. Image courtesy of Dr. Farshid Sepehrband and Arthur Toga, PhD.At the Mayo Clinic, the No. 1 application for 7-tesla MRI is for patients with seizures. In fact, seizure imaging is driving all referrals for 7 tesla, Welker said.
"If we can find the abnormality in the brain of a patient having seizures and the brain can be surgically resected, we can potentially cure a patient of their seizures," he said. "Many of these little areas that cause seizures are focal cortical dysplasias that tend to be very small and very subtle. Many of them are literally invisible on 1.5-tesla and 3-tesla scanning."
Vascular imaging is also improved for both arteries and veins in terms of blood vessels within the brain. The high-field magnet is "extremely good for sorting out small aneurysms and trying to determine whether an abnormality seen on a 1.5-tesla scanner or a 3-tesla scanner is an aneurysm or not," Welker said.
MSK at 7T
 Dr. Kimberly Amrami from the Mayo Clinic.
Dr. Kimberly Amrami from the Mayo Clinic.As for the knee, the Mayo Clinic is using 7-tesla imaging to better view cartilage transplants and determine whether patients' knees are reverting to normal or if there is evidence of scarring. The knee coil also is used by clinicians to image wrists, feet, and ankles.
"The big benefit is the way we see tiny structures that we want to distinguish from surrounding tissue and better characterize them," said Dr. Kimberly Amrami, chair of the division of musculoskeletal radiology at Mayo. "That is where [7 tesla] does its best work -- when we need to see something that requires ultrahigh resolution that we cannot get to see on 1.5 or 3 tesla in any kind of reasonable imaging time frame."
However, 7 tesla is not yet appropriate for routine knee imaging. Amrami said clinicians are dealing with "some of the artifacts that are quite a bit worse related to the higher field strength and are not a substitute for what we are seeing on our 3-tesla scanners. So [7 tesla] is definitely more useful for specific patients who have specific problems."
Since the installation of the 7-tesla scanner at USC last year, clinicians have been applying pulse sequences in use on their 3-tesla scanners to the 7-tesla device for research purposes. In one recent case, they scanned a patient with a pituitary tumor under a research protocol using 7 tesla.
The scan data were given to the neurosurgeon who was "impressed by the fact that he could see the tumor in 7 tesla that he could not see at lower field strength," said Arthur Toga, PhD, from USC's Stevens Neuroimaging and Informatics Institute. "That gave him a distinctive presurgical planning advantage prior to the procedure and gave us a good indication of the utility of the high field in a clinical scenario."
Patient comforts
Thus far, patients at all three facilities appear to be tolerating the greater magnet strength quite well, with a few cases of temporary dizziness. To help alleviate that issue, Siemens slowed down the speed at which patients entered and exited the Terra's magnet bore.
 Dr. Srinivasan Mukundan, PhD, from BWH.
Dr. Srinivasan Mukundan, PhD, from BWH."The field strength is so high that it impacts ion flows in the inner labyrinth of the ear," Welker said. "Consequently, patients who are being put into the scanner often feel like they are moving on a curve, even though the table is moving in a straight line. This is most commonly a very transient phenomenon that lasts only a minute or two."
At Brigham and Women's, no one has complained of adverse side effects from the scan, Mukundan said. Clinicians there have minimized the potential for side effects by placing patients into and removing them from the scanner slowly.
"Every scanner has a certain rate of people who cannot complete the requirements," he added. "Sometimes people feel claustrophobic or are in pain and cannot stay still."
Indeed, claustrophobia can be an issue with the current 7-tesla scanner design. The scanner has a 60-cm opening and a rather long bore, which can seem especially tight for some patients. Then again, lower-field-strength scanners had the same problem when they were first introduced in radiology departments, before wider and more open designs were developed.
"Our first 3-tesla scanner was 55 cm [in diameter] and had a very long bore, so this is something we experienced back then, too," Mayo's Amrami said. "I think we are at a point of evolution with 7 tesla, as early adopters, and things will continue to evolve technically to improve that patient experience."
Safety first
Clinicians are also extremely careful about patients with implants and which accessories may or may not be conducive to 7-tesla scans. When the scanner was first installed at the Mayo Clinic, clinicians did not scan patients with any sort of implanted device, with the exception of dental amalgam, Welker said.
 Arthur Toga, PhD, from USC.
Arthur Toga, PhD, from USC."Over the past year, our physicists, technologists, and MR safety committee have worked hard to understand what is safe and what is not safe to put in a 7-tesla MRI scanner," he said.
While the number of items on that safe list has increased over the past year, it remains a small subset of implants that are safe for 3 tesla.
USC's current policy is not to image any patient with any sort of implant using 7 tesla, Toga said. Frank Shellock, PhD, an adjunct professor of clinical physical therapy at USC, is leading the effort to investigate the safety of implants at the higher magnet strength.
The road ahead
As for the future, USC's Toga predicted that 7-tesla MRI will be applied to all tertiary care situations where clinicians need to see anomalies that otherwise cannot be detected at lower magnet strengths.
"It is an expensive machine and has some environmental requirements that are not typical for many hospitals," he said. "I don't think we will see widespread adoption of that field strength in every single hospital, but certainly in academic medical centers. People will realize the potential for utilizing this in cases where it is warranted, especially in neurosurgical cases and in the knee."
In the meantime, expect radiology departments to ease into 7-tesla MRI.
"It is always an iterative process when we go to a new technology," BWH's Mukundan said. "We want to be very careful in how we implement it, release it, and learn how to optimize the imaging and utilize the results. We have worked closely with our clinical colleagues in the neuroscience area to establish the protocols and review the results to correlate what we're seeing clinically."