Cardiac MRI's ability to noninvasively provide a microscopic view of living tissue plays a critical role in helping clinicians differentiate between symptoms of heart disease and cocaine-induced cardiac abnormalities, according to a study published June 13 in Radiology: Cardiothoracic Imaging.
Cocaine use can lead to myocardial infarction, acute myocarditis, and chronic cardiomyopathy, but those conditions also can occur from situations that aren't related to drug abuse, which makes a cause-and-effect diagnosis challenging.
This is where cardiac MRI is beneficial: Italian researchers reviewed previous studies on the use of cardiac MRI to evaluate cocaine abuse and found that the modality is quite proficient in identifying the drug's effects on the cardiovascular system and the degree of resulting damage.
"Cardiac MRI's ability to distinguish between the different cardiac manifestations of cocaine abuse is important because they all have different patterns," said co-author Dr. Marco Francone, PhD, in a statement. "Even though all these pathologies have cocaine abuse as primary cause, the myocardial damage and, therefore, clinical course are completely different, ranging from complete recovery to heart failure."
Cocaine abuse is a significant public health problem around the world. An estimated 1.5 million cocaine users age 12 years and older were recorded in the U.S. in 2014, according to the National Survey on Drug Use and Health. And as the study authors note, "Cocaine consumption in 2016 is estimated to have increased by almost 7% from the previous year, and global consumption is increasing among individuals of every socioeconomic strata."
The heart is one of the organs most affected by cocaine abuse. Cocaine can lead to uncontrolled stimulation of the heart's rhythm, arterial hypertension, inflammation or enlarging of the heart muscle (also known as cardiomyopathy), and other adverse conditions that worsen as the drug abusers age.
More than 500,000 cocaine users come to emergency rooms complaining of chest pains annually, but only 6% of those cases are myocardial infarction. With the help of cardiac MRI, clinicians can distinguish between cocaine-induced heart attacks and cardiac events that aren't related to drug abuse.
For example, in cases of noncocaine-related acute myocardial infarction, plaque rupture is associated with myocardial necrosis. By contrast, cardiac MRI discounts any plaque rupture or hemorrhage and often results in a diagnosis of an imbalance of oxygen to the heart in cases of chest pain.
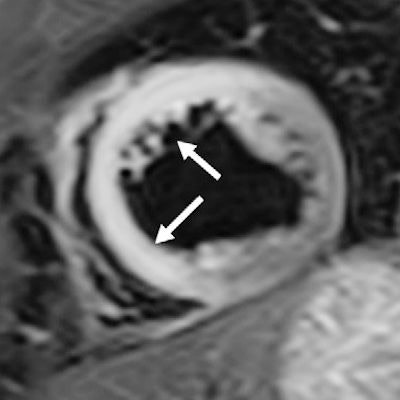
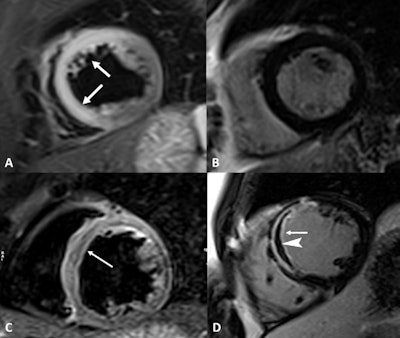 Cardiac MR images acquired from a 44-year-old woman with acute chest pain and chronic cocaine abuse for more than 10 years. Short-axis T2-weighted short tau inversion-recovery (STIR) image (A) demonstrates the presence of transmural edema (arrows) in the anteroseptal and inferoseptal myocardial segments (left descending artery's vascular territory). The late gadolinium enhancement (LGE) sequence in the same cardiac plane (B) did not show gadolinium deposition inside the myocardium. MR images also show an anteroseptal infarction with microvascular obstruction in a 38-year-old man with long-standing abuse of cocaine and troponin elevation. Edema (C) is in the anteroseptal wall (arrow). The short-axis LGE sequence (D) highlights transmural hyperintensity of the anteroseptal wall (arrow) with linear hypointensity (arrowhead) inside the microvascular obstruction. Images courtesy of Radiology: Cardiothoracic Imaging.
Cardiac MR images acquired from a 44-year-old woman with acute chest pain and chronic cocaine abuse for more than 10 years. Short-axis T2-weighted short tau inversion-recovery (STIR) image (A) demonstrates the presence of transmural edema (arrows) in the anteroseptal and inferoseptal myocardial segments (left descending artery's vascular territory). The late gadolinium enhancement (LGE) sequence in the same cardiac plane (B) did not show gadolinium deposition inside the myocardium. MR images also show an anteroseptal infarction with microvascular obstruction in a 38-year-old man with long-standing abuse of cocaine and troponin elevation. Edema (C) is in the anteroseptal wall (arrow). The short-axis LGE sequence (D) highlights transmural hyperintensity of the anteroseptal wall (arrow) with linear hypointensity (arrowhead) inside the microvascular obstruction. Images courtesy of Radiology: Cardiothoracic Imaging."The real challenge is early diagnosis of cocaine-induced cardiomyopathy and, in particular, its asymptomatic stage," Francone said. "Early diagnosis can indeed have a significant impact on clinical outcome, preventing evolution to heart failure."
Typically, the diagnostic workup of cocaine abuse includes the person's clinical and drug use history, laboratory tests, an electrocardiogram, a stress test, an imaging modality such as cardiac MRI, and coronary angiography. From there, based on their literature review, the researchers recommend that clinicians initially investigate both the patient's acute and chronic conditions, with a primary focus on biventricular function to determine how well the heart is pumping blood to the rest of the body and to help identify different phases of chronic cardiomyopathy.
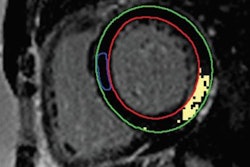
More specifically, "cine sequences ... performed on the entire short-axis, four-chamber, and long-axis planes are crucial for evaluation of ventricular function abnormalities," they added. Tissue characterization should include STIR and T2 mapping for edema, as well as T1 mapping, extracellular volume, and LGE sequences to evaluate for fibrosis and necrosis. To diagnose myocarditis, T2-based imaging and T1-based MR imaging criteria are both necessary.


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











