The ability of resting-state functional MRI (fMRI) to pinpoint reduced brain connectivity in individuals with mood disorders could help clinicians detect people who might become suicidal, according to a study published October 10 in Psychological Medicine.
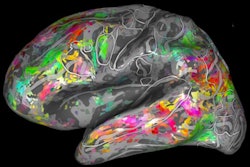
Researchers from the University of Utah Health and the University of Illinois at Chicago used fMRI to acquire brain images of network connectivity in 212 young adults while they calmly rested. The fMRI scans revealed a lack of connectivity in brain networks associated with cognitive control and impulsivity among subjects with mood disorders and a history of suicide attempts.
"These results suggest that individuals with a history of suicide-related behavior in the context of mood disorders may show reliably distinct patterns of intrinsic network connectivity, even when compared to those with mood disorders without suicide-related behavior," wrote the authors, led by Scott Langenecker, PhD, professor of psychiatry at the University of Utah Health. "Resting-state fMRI is a promising tool for identifying subtypes of patients with mood disorders who may be at risk for suicidal behavior."
Previous research has linked certain brain circuits with mood disorders. The culprits include the cognitive control network, which is associated with executive function, problem-solving, and impulsivity; the salience and emotional network, which handles emotion processing and regulation; and the default mode network, which is active during self-focused thought. These studies, however, have focused primarily on depression.
"Little is known about the neural substrates of suicide risk in mood disorders," Langenecker and colleagues wrote. "Improving the identification of biomarkers of suicide risk, as indicated by a history of suicide-related behavior, could lead to more targeted treatments to reduce risk."
To that end, the researchers enrolled into the study 130 young adults, all of whom had experienced mood disorders but were in remission. The cohort was then divided into three groups:
- 18 subjects who also had a history of suicide-related behavior and a previous suicide attempt
- 60 subjects with a history of suicidal thoughts but no suicide-related behavior
- 52 subjects with no suicidal thoughts or suicide-related behavior
The analysis also included 82 healthy controls subjects for comparison. Functional MRI scans were performed to image and compare the groups' brain connectivity within and between the brain's neural networks.
"For risk factors involved in suicide, the tasks we have to measure are pretty nonspecific and inexact," Langenecker noted in a statement. "If we go to the level of the resting-state networks, we're actually asking the brain to tell us which brain networks and connections are most relevant."
The fMRI results showed that individuals with mood disorders and a history of suicide attempts showed less connectivity in the cognitive control network and between the cognitive control network and the default mode network, compared with the other three groups. The most significant differences in functioning connectivity were in the frontoparietal regions, even when compared with subjects with mood disorders and a history of suicidal thoughts but no attempts. Connectivity dysfunction in some of these same brain regions was still evident on follow-up fMRI scans one to four months later.
The researchers noted that their work is still in its early stages and will need replication and validation in a longitudinal study with a larger cohort. They suggested taking baseline brain circuit readings and following up to check on participants' conditions. This approach also might provide additional information on which risk factors to monitor and when to intervene.