Using MRI data for 3D-printed orbital models can help clinicians plan surgery to treat blowout fractures, according to a study published in the April issue of the International Journal of Oral and Maxillofacial Surgery.
The findings offer patients and surgeons a radiation-free alternative to CT, which has long been the gold standard for staging orbital fracture surgery, wrote a team led by Dr. Thomas Cooper of Royal Perth Hospital in Australia.
"[Our] research suggests that MRI is comparable to CT when imaging isolated orbital blowout fractures," the group wrote.
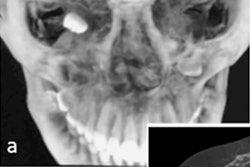
Orbital fractures are common traumatic injuries to the orbital floor, most often caused by blunt trauma, the group wrote. Imaging is used at a variety of stages for the condition, with CT as the go-to modality for this application. CT has some downsides, however, including the potential for cataracts as the result of repeated radiation exposure.
That's why interest in using MRI to create preoperative, 3D-printed reconstructive plates has increased, according to Cooper and colleagues.
"MRI has been proposed as an alternative to CT scanning for the diagnosis and review of orbital fractures multiple times in the literature over the years," the group wrote. "However, its efficacy in preoperative planning has only recently been suggested [by researchers] who demonstrated that accurate 3D virtual models may be constructed from MRI data of intact orbits."
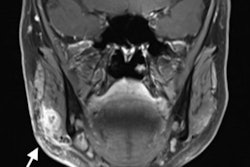
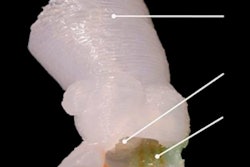
Cooper's team sought to test the accuracy of 3D-printed models using MRI data for the preoperative construction of plates used to treat orbital blowout fracture. The MRI information had to be segmented -- a process of manually delineating the bony boundaries in each slice of an MRI scan, according to the authors (International Journal of Oral and Maxillofacial Surgery, April 2020, Volume 49:4, pp. 483-490).
The study included six orbits and seven fractures. The researchers found high congruence between the fracture margins on CT and MRI: Average deviation ranged from 0.51 mm to 1.13 mm (overall mean, 0.85 mm). They also found no significant difference between plates constructed according to the 3D models of the fractures using CT or MRI data.
"This research suggests that MRI is comparable to CT when imaging isolated orbital blowout fractures, as evidenced by all blowout fractures maintaining an average fracture boundary deviation from the gold standard of CT of 1.13 mm or less," the team wrote.
MRI did have a limitation, Cooper and colleagues noted: Segmentation time was considerable, taking eight hours on average. Nonetheless, the study findings suggest that MRI could be a useful modality in the preoperative 3D printing of reconstruction plates for orbital fractures.
"MRI is capable of producing highly accurate biomodels of the bony orbit and ... these biomodels are suitable to produce highly accurate orbital reconstruction plates in the setting of orbital blowout fracture," the investigators concluded. "The segmentation time will need to be improved prior to routine clinical use becoming feasible; with advances in technology this may not be far away."