A lesion classification scheme named after breast MRI pioneer Dr. Werner Kaiser may help prevent anywhere from 45% to 72.5% of unnecessary breast biopsies in high-risk patients, Austrian researchers have found. The tool also refutes the notion of benign-appearing cancers.
The research team led by Dr. Pascal Baltzer from the Medical University of Vienna examined 183 histologically proven suspicious breast MRI lesions classified as BI-RADS 4. Readers blinded to the histopathology evaluated all lesions according to the Kaiser score, and the clinical decision-support tool demonstrated sensitivity between 95.1% and 97.6% for all lesions (European Radiology, June 6, 2020).
"We think it is safe to conclude that the Kaiser score can without a doubt be safely applied to downgrade mass lesions but caution should be used when interpreting nonmass lesions and foci," Baltzer and colleagues noted.
What is the Kaiser score?
The Kaiser score is named after breast MRI pioneer Dr. Werner Kaiser, who developed MR mammography in 1983 in partnership with Siemens Healthcare. He died in Bonn, Germany in December 2013.
The classification uses a small set of morphological and dynamically relevant features that were chosen by machine-learning methodology. The features include the following:
- Presence of spiculations/root sign
- Enhancement kinetics
- Lesion margin
- Internal enhancement pattern
- Ipsilateral edema
The Kaiser score's three-step flowchart (which may also be accessed online) indicates probabilities of malignancy, ranging from 1 to 11, with 11 being the highest probability. Kaiser scores below 5 are considered benign, while histological workup is mandatory for higher scores.
The Austrian researchers initiated their study due to resolve the perception that there are differences in the appearance of breast cancer lesions between high-risk and average-risk women, according to Baltzer.
"It bothered me that colleagues considered breast cancer lesions in high-risk patients to appear different on MRI as compared with those detected in 'regular' patients," he told AuntMinnie.com. "Given the biological basis of breast cancer, this is quite counterintuitive."
Cancer growth leads to typical changes both in microstructure and vascularization that provide diagnostic clues as evident as any margin spiculation, and thus it's important to look at the whole picture, not just one diagnostic criterion, he added.
"I am astonished by authors having coined the term 'fibroadenoma-like cancers,' as the resemblance is quite farfetched. I could call an orange a planet-like fruit for comparison and just ignore size, texture, color, surface water, magnetic field, etc.," Baltzer continued. "If you look into the literature, the term and the notion of benign-appearing cancers in high-risk women is actually not common in original research -- it is just an idea gone viral, as it sounds logical."
He said many women undergo unnecessary biopsies because the diagnostic tools available are not used how they are intended, and radiologists are afraid of missing "fibroadenoma-like" cancers. Could the Kaiser score reduce the number of unnecessary biopsies?
To test the hypothesis, the researchers included high-risk women with the BRCA-1/BRCA-2 gene, or those with a family history of the disease. All patients in the study underwent annual screening with two-view mammography, ultrasound, and MRI every 12 months with a maximum interval of one month between the modalities.
After exclusions, the study consisted of 183 breast MRI-visible lesions classified as BI-RADS 4 in 159 patients. These lesions were biopsied using image guidance or surgically biopsied. All lesions underwent histopathological analysis. Histopathology revealed 142 benign and 41 malignant lesions.
Three readers blinded to the final histopathological diagnosis scored the lesions using the Kaiser score. Scores of 4 or greater required biopsy. For all lesions, the Kaiser score's accuracy represented by the area under the curve (AUC) ranged between 86.5 and 90.2. The Kaiser score demonstrated high sensitivity: between 95.1% and 97.6% for all lesions, but it worked best in mass lesions. Using the 4 or greater threshold, the Kaiser score could have potentially avoided 64 (45.1%) to 103 (72.5%) unnecessary biopsies in 142 benign lesions.
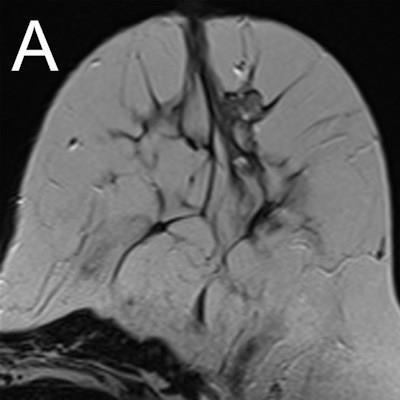
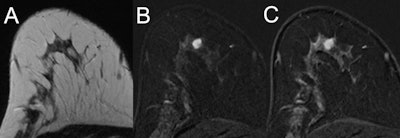 MRI of a 47-year-old high-risk patient (A, T2-weighted; B and C, subtracted early and late contrast-enhanced, T1-weighted images) shows a rather circumscribed mass lesion with heterogeneous internal enhancement and washout, corresponding to a Kaiser score of 8. Histology revealed a luminal-type invasive lobular cancer, B5b. Images courtesy of European Radiology.
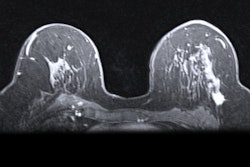
MRI of a 47-year-old high-risk patient (A, T2-weighted; B and C, subtracted early and late contrast-enhanced, T1-weighted images) shows a rather circumscribed mass lesion with heterogeneous internal enhancement and washout, corresponding to a Kaiser score of 8. Histology revealed a luminal-type invasive lobular cancer, B5b. Images courtesy of European Radiology.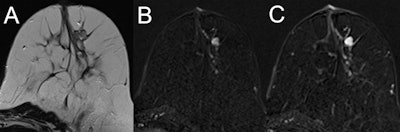 MRI of a 39-year-old high-risk patient (A, T2-weighted; B and C, subtracted early and late contrast-enhanced, T1-weighted images) shows a circumscribed mass lesion with heterogeneous internal enhancement and persistent signal increase, corresponding to a Kaiser score of 1. Note the fibroadenoma-like T2-weighted correlate (A). Histopathology revealed a fibroadenoma, B2.
MRI of a 39-year-old high-risk patient (A, T2-weighted; B and C, subtracted early and late contrast-enhanced, T1-weighted images) shows a circumscribed mass lesion with heterogeneous internal enhancement and persistent signal increase, corresponding to a Kaiser score of 1. Note the fibroadenoma-like T2-weighted correlate (A). Histopathology revealed a fibroadenoma, B2."I can warmly recommend the Kaiser score to everyone, as it forces the reader to assess all relevant diagnostic criteria before coming to a conclusion," Baltzer noted. "Gut-feeling decisions (that regularly happened to me) are avoided."
Part of the reason he makes this recommendation is that the Kaiser score relies on generally recommended standard breast MRI protocols, the type of scanner used is irrelevant, and the score is also helpful for less-experienced radiologists.
Can the Kaiser score be refined to integrate clinical or mammographic information? That's what the Viennese group is tackling next.