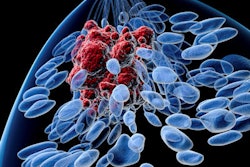
Hormone receptor-positive breast cancers are on the rise in the U.S., according to new data published on August 17 in JAMA Network Open. At the same time, rates of triple-negative cancers have fallen for some groups of women in recent years.
The new data comes from an analysis of breast cancer subtypes among more than 300,000 women diagnosed with invasive breast cancer in the past decade. While more luminal A and B breast cancers are getting diagnosed, the rates vary by age and race/ethnicity.
"This cross-sectional study found that between 2010 and 2016, hormone receptor-positive breast cancer subtypes increased for many racial/ethnic and age groups, with the largest and most consistent increases observed for luminal B breast cancer in non-Hispanic white and Hispanic women," wrote the authors, led by Teofilia Acheampong, PhD, from the Mailman School of Public Health at Columbia University.
Breast cancer subtype is important for treatment planning, prognosis estimates, and even determining risk factors. Some preliminary research has suggested that the prominence of certain breast cancer subtypes has changed in recent years, so the researchers investigated this trend using the most up-to-date data they had at their disposal.
Their cross-sectional analysis utilized data from the U.S. Surveillance Epidemiology and End Results (SEER) database, which includes patient information from 18 cancer registries. The final analysis included 320,124 women diagnosed with invasive breast cancer between 2010 and 2016.
The vast majority of the women (73%) had luminal A breast cancers, which tend to grow slowly and have the best prognosis. Another 11% of women had luminal B cancers, 11% had triple-negative cancers, and 5% had ERBB2-enriched cancers, also known as HER2-enriched cancers.
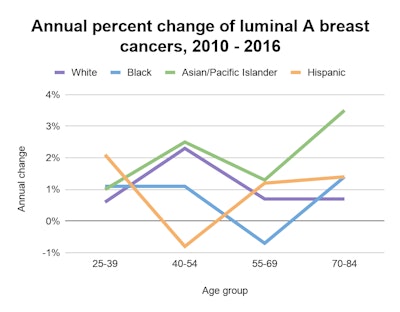
Incidence rates of luminal A cancers increased during the study period. Incidence rates rose by 2.3% annually for white women ages 40 to 54 until 2014 and by 4.9% annually for Black women ages 55 to 69 until 2012. Rates also increased for Asian/Pacific Islander women ages 40 to 54.
The slope of luminal A cancers also increased significantly during the study period. It was the only cancer subtype to experience a significant change in slope, the authors noted.
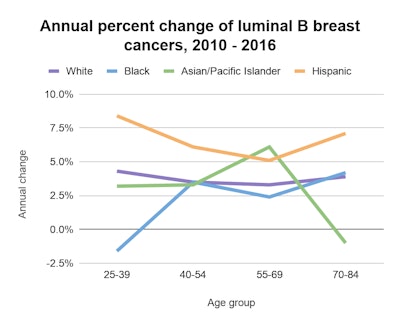
For luminal B cancers, the incidence rate increased for white women and Hispanic women of all ages, with the largest increase occurring in women ages 25 to 39. The researchers also noted a 6.1% annual increase in luminal B cancers for Asian and Pacific Islander women ages 55 to 69.
The incidence rate of HER2/ERBB2-enriched cancers only increased for white women ages 25 to 39. Meanwhile, triple-negative cancers decreased by 2.3% annually for white women ages 40 to 54 and by 3.6% annually for white women ages 55 to 69. Triple-negative cancer rates also decreased by 1.4% annually for Black women.
While the authors do not know what is causing the fluctuations in cancer subtypes, they noted the findings were consistent with other population-based analyses. They hope future research will continue to analyze breast cancer subtype trends, especially how the changes reflect risk in populations typically not recommended for breast screening.
"Changes in incidence trends for particular subtypes, such as ERBB2-positive breast cancers, that are consistent across all age groups or that are present for younger age
groups who are not likely participating in breast cancer screening suggest a real change in risk for those subtypes rather than greater detection through increasing screening over time," they wrote.