Swiss researchers have found that although routine knee MRI scans of adolescents often show incidental irregularities in the distal femur bone that may be confused with more serious conditions, these are typically benign and can be tracked as such, according to a study published June 16 in Radiology.
The study results should help clinicians better recognize these injuries, called distal femoral cortical irregularities (DFCIs) -- and therefore help young people avoid invasive diagnostic procedures, said lead author Dr. Christoph Stern of the University of Zurich, in a statement released by the RSNA.
"DFCIs are benign lesions, and occurrence around the knee joint is associated with repetitive mechanical stress to the attachment sites of tendons into bone," he said. "DFCI should not be mistaken for malignancy and are not associated with intraarticular damage."
Cortical irregularities at the posterior distal femur are common findings in adolescents, but what causes them has been unclear. There have been no studies investigating the association between mechanical stress to the knee and the development of DFCIs, according to the researchers.
Stern's group sought to assess the prevalence of DFCIs at different tendon attachment sites in 105 young competitive alpine skiers compared to 105 nonskiers (mean age for both groups, 14). Each participant underwent unilateral, unenhanced knee MRI exams.
Two radiologists assessed the exams for the presence of DFCIs at the femoral attachment of the medial or lateral head of the gastrocnemius muscle and the attachment between the adductor magnus muscle and the inner thigh and/or femur. Stern and colleagues then evaluated tendon attachment position and MRI findings for an association with DFCI.
There were 61 distal DFCIs in the skier group (58%) compared with 28 in the control group (27%). The authors found the following distribution patterns for the DFCIs.
| Distribution patterns of DFCIs in young skiers and nonskiers | ||
| Location | Skiers | Nonskiers |
| Medial head of gastrocnemius muscle | 95.2% | 92.8% |
| Lateral head of gastrocnemius muscle | 4.8% | 3.6% |
| Adductor magnus tendon attachment site | 0% | 3.6% |
The group also found the following:
- Comparable mean size of medial head gastrocnemius muscle-related DFCIs in skiers and nonskiers, at 3.7 mm and 3.4 mm, respectively
- No difference in the medial head gastrocnemius muscle tendon attachment position in knees with DFCI and those without
- Significant association between increased signal intensity of the medial head gastrocnemius muscle tendon with medial head gastrocnemius muscle-related DFCI in both groups
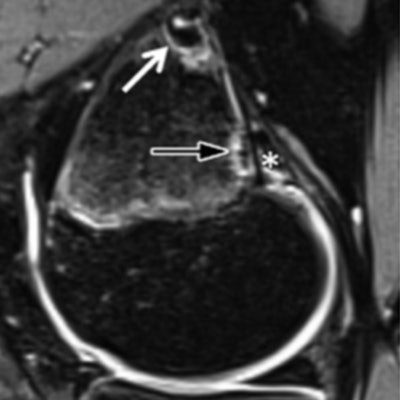
![Images show examples of (a-d) DFCI at the tendon attachment of the medial head of the gastrocnemius muscle [MHG] and (e, f) knees without DFCI. Sagittal (a) and axial (b) fat-suppressed T2-weighted MRI scans in a 14-year-old female competitive skier show a 5-mm DFCI (arrow) at the distal MHG attachment (*). (c) Sagittal fat-suppressed T2-weighted MRI scan in another 14-year-old female competitive skier shows simultaneous DFCIs at the proximal (8 mm; white arrow) and distal (4 mm; black arrow) part of the MHG tendon attachment (*). (d) Sagittal fat-suppressed proton density-weighted MRI scan in a 14-year-old female control participant shows a 4-mm DFCI (arrow) at the distal MHG attachment (*). Sagittal fat-suppressed proton density-weighted MRI scans in 15-year-old female control participant (e) and 15-year-old male control participant (f) without a DFCI for comparison. The broad and fan-shaped appearance of the proximal MHG tendon (*) is especially well visualized in (f) because of edematous demarcation after knee trauma. Caption and images courtesy of the RSNA.](https://img.auntminnie.com/files/base/smg/all/image/2020/06/am.2020_06_13_00_30_6352_2020_06_16_MRI_alpine_ski_figure_4_20200613001147.png?auto=format%2Ccompress&fit=max&q=70&w=400) Images show examples of (a-d) DFCI at the tendon attachment of the medial head of the gastrocnemius muscle [MHG] and (e, f) knees without DFCI. Sagittal (a) and axial (b) fat-suppressed T2-weighted MRI scans in a 14-year-old female competitive skier show a 5-mm DFCI (arrow) at the distal MHG attachment (*). (c) Sagittal fat-suppressed T2-weighted MRI scan in another 14-year-old female competitive skier shows simultaneous DFCIs at the proximal (8 mm; white arrow) and distal (4 mm; black arrow) part of the MHG tendon attachment (*). (d) Sagittal fat-suppressed proton density-weighted MRI scan in a 14-year-old female control participant shows a 4-mm DFCI (arrow) at the distal MHG attachment (*). Sagittal fat-suppressed proton density-weighted MRI scans in 15-year-old female control participant (e) and 15-year-old male control participant (f) without a DFCI for comparison. The broad and fan-shaped appearance of the proximal MHG tendon (*) is especially well visualized in (f) because of edematous demarcation after knee trauma. Caption and images courtesy of the RSNA.
Images show examples of (a-d) DFCI at the tendon attachment of the medial head of the gastrocnemius muscle [MHG] and (e, f) knees without DFCI. Sagittal (a) and axial (b) fat-suppressed T2-weighted MRI scans in a 14-year-old female competitive skier show a 5-mm DFCI (arrow) at the distal MHG attachment (*). (c) Sagittal fat-suppressed T2-weighted MRI scan in another 14-year-old female competitive skier shows simultaneous DFCIs at the proximal (8 mm; white arrow) and distal (4 mm; black arrow) part of the MHG tendon attachment (*). (d) Sagittal fat-suppressed proton density-weighted MRI scan in a 14-year-old female control participant shows a 4-mm DFCI (arrow) at the distal MHG attachment (*). Sagittal fat-suppressed proton density-weighted MRI scans in 15-year-old female control participant (e) and 15-year-old male control participant (f) without a DFCI for comparison. The broad and fan-shaped appearance of the proximal MHG tendon (*) is especially well visualized in (f) because of edematous demarcation after knee trauma. Caption and images courtesy of the RSNA.Stern and colleagues hope the findings will help young patients with DFCI avoid invasive diagnostic procedures.
"Due to the benign, usually asymptomatic, and, over time, self-limiting character of typical DFCIs at the attachment sites of tendons, invasive diagnostic procedures such as biopsies should be avoided," the team concluded. "However, follow-up with MRI might be justified, especially in the rare case of a symptomatic presentation."