Adding textural analysis to breast MRI appears to boost the modality's accuracy when it comes to differentiating malignant from benign axillary lymph nodes in women with breast cancer, according to a study published July 4 in the Journal of Breast Imaging.
And better node characterization translates into better patient care, wrote a team led by Dr. Rifat Wahab of the University of Cincinnati Medical Center in Ohio.
"Using [textural analysis], the radiologist can obtain quantitative information that may not be visible to the human eye on individual nodes that can assist with determining the malignant status of specific lymph nodes," the authors wrote. "Clinicians can utilize this information from MRI [textural analysis] to develop more detailed axillary management plans for patients."
Better treatment
Assessing the axilla is a key part of developing a management and treatment plan for breast cancer patients, and it typically begins with ultrasound. Women often undergo ultrasound-guided biopsy of abnormal nodes. Traditionally, patients with nodes positive for cancer have been staged with node dissection; however, these dissections are associated with increased risk of lymphedema.
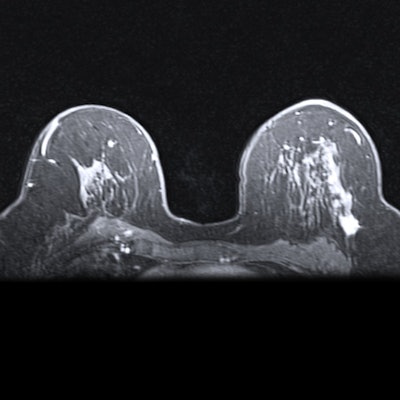
In an effort to develop other approaches for managing breast cancer patients that don't involve lymph node dissection, clinicians have turned to MRI to evaluate the axilla. MRI's accuracy for this application has been moderate, with a sensitivity of 70% and a specificity of 90%, but adding radiomics such as shape, size, and texture can improve the modality's performance.
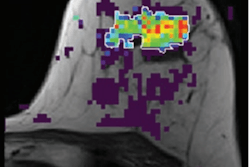
For their study, Wahab and colleagues particularly investigated texture (the differences in grayscale of pixels within a region of interest, with higher rates of change in pixel intensity translating to rough textures, i.e., malignant nodes, and lower rates of change translating to smooth textures, i.e., benign nodes).
"Management of the axilla has changed over the last few years to a more conservative approach which has decreased the morbidity women face after axillary surgery, and imaging plays a key role in identifying abnormal lymph nodes during the staging process," Wahab told AuntMinnie.com via email. "However, there are abnormalities not visible to the human eye on imaging and that is where radiomics comes into play."
The investigators analyzed 23 biopsy-proven malignant lymph nodes and 24 benign nodes in 43 women who underwent ultrasound-guided biopsy and contrast-enhanced breast MRI between January 2015 and December 2018. The MRI exams also included textural analysis of the axillary lymph nodes with the following sequences:
- 3D dynamic contrast-enhanced T1-weighted fat-suppressed
- 3D delayed contrast-enhanced T1-weighted fat-suppressed
- T2-weighted fat-suppressed
The researchers compared the measures used to evaluate the textural analysis with pathology results and calculated area under the receiver operating curve (AUC) to assess the ability of textural analysis to distinguish between cancerous and noncancerous nodes by sequence.
The team found that the contrast-enhanced T1-weighted fat-suppressed sequence was the most effective for distinguishing between malignant and benign nodes in terms of AUC; in this sequence, kurtosis was the most prominent textural analysis parameter, with a P value of < 0.0001.
| MRI textural analysis for distinguishing between malignant and benign axillary nodes | |||
| Measure | 3D dynamic contrast-enhanced T1-weighted fat-suppressed | 3D delayed T1-weighted fat-suppressed | T2-weighted fat-suppressed |
| AUC | 0.70-0.84 | 0.84-0.93 | 0.68-0.74 |
| Sensitivity | 57%-83% | 78%-87% | 50%-80% |
| Specificity | 68%-96% | 76%-88% | 64%-88% |
Adding textural analysis to breast MRI offers an effective way to boost its accuracy, particularly in the 3D dynamic contrast-enhanced T1-weighted fat-suppressed sequence, the team wrote.
"The results of our study are important, as they indicate that MRI [textural analysis] has the potential to differentiate between malignant and benign axillary lymph nodes," Wahab and colleagues wrote.
More to explore
There's more to explore when it comes to evaluating the benefits of adding textural analysis to breast MRI, according to Wahab.
"Our study lays a foundation upon which to build future research," she said. "A future goal would be to see if [textural analysis] can detect micro-metastasis, which can further aid with determining an axillary management plan for patients diagnosed with breast cancer."