Breast density calculations derived from mammograms can be used to predict lymphedema risk in breast cancer survivors. The study, published on November 11 in JAMA Network Open, was the first to peg breast density as a prognostic factor for lymphedema, according to the authors.
Research has already established body mass index (BMI) as a risk factor for lymphedema occurrence and severity. But BMI is only a surrogate for other risk factors, such as fat deposition and high lipid levels.
When the team behind the study looked for new ways to better personalize lymphedema risk assessment, they realized all patients with breast cancer underwent a diagnostic mammogram that includes breast density results. The resulting analysis proved that breast density could serve as an alternative to BMI for fat measurements.
"In this study, a new prognostic patient factor for lymphedema was identified: mammographic breast density, a more direct measure of adiposity than BMI, which is calculated from height and weight," wrote the authors, led by Dr. Jennifer Yin Yee Kwan, a radiology oncology resident at the University of Toronto.
Lymphedema is a disabling side effect associated with treatment for breast and other cancers. In the new prognostic study, the researchers looked for individual factors that could better predict lymphedema risk to support earlier interventions and, ultimately, better patient outcomes.
The study included electronic health record data for 373 women referred to a survivorship program at the University of Toronto after completing curative treatment for breast cancer. The program provided care specifically to cancer survivors with lymphedema, fatigue, function, and mobility issues.
After analyzing almost two dozen data points, the authors discovered that mammographic breast density was one of five characteristics significantly associated with lymphedema volume. Other significant factors included age, BMI, number of pathological lymph nodes, and axillary lymph node dissection.
A model that used all five factors performed best at predicting lymphedema occurrence and severity, achieving an area under the curve (AUC) of 0.81 for mild-to-severe lymphedema and 0.86 for severe lymphedema in a training cohort of two-thirds of the patients. In the remaining validation cohort, the model netted an AUC of 0.72 and 0.83, respectively.
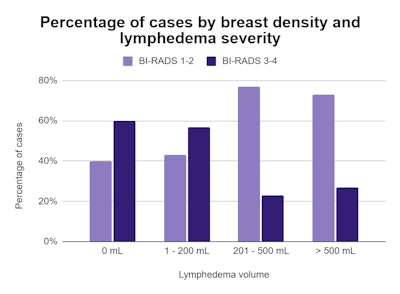
Furthermore, when the authors plotted the cases on a matrix, they found a significant association between women with the fattiest breast tissue (BI-RADS 1) and disease severity. However, the findings dropped out of statistical significance for women with denser breast tissue.
"The study revealed that fatty breasts concurred with worse lymphedema, and on multivariate analysis, breast density added an independent prognostic value beyond BMI," the authors wrote.
While the findings demonstrated the value of mammographic breast density as a prognostic factor for lymphedema, the reason behind this relationship is not so clear. The authors postulated that the association could be explained by adipose tissue dysfunction in the breast and compromised lymphatic vasculature.
In an invited commentary, Dr. Maggie DiNome added that the relationship between breast density and BMI is complex. However, she also said the findings are clinically relevant and, if further validated, could provide patient-specific variables to improve patient care.
"The ability to better predict the risk of lymphedema in these patients is essential not only for appropriate counseling but also for earlier identification and intervention to mitigate the risk of developing this potentially disabling complication," wrote DiNome, chief of breast surgery and system director of breast health for University of California, Los Angeles.