Patients with COVID-19 are more likely to have thromboembolism than those without the disease, according to a report published September 22 in the American Journal of Roentgenology.
The study findings suggest that radiologists who identify thrombembolic findings on imaging should raise the alarm for COVID-19, wrote a team led by Dr. Bari Dane of NYU Langone Medical Center in New York City.
"Although COVID-19 typically presents with respiratory symptoms, patients may not experience symptoms or may develop multiple-organ dysfunction syndrome (MODS)," the group wrote. "MODS in COVID-19 may result from hypercoagulability ... some reports have described deep venous thrombosis and pulmonary embolism. Some patients may have hypercoagulability, often with extremely elevated coagulation and inflammatory markers. Radiologists may not be aware of this potential complication of COVID-19, although reports are emerging in the literature."
For their study, Dane and colleagues sought to describe arterial and venous thromboembolism in the abdomen, pelvis, and lower extremities in patients with coronavirus disease (COVID-19). The work included 82 COVID-19 patients who underwent abdominal ultrasound or CT who were compared to 82 patients without the disease for thromboembolism and solid-organ infarction.
Of the COVID-19 patient cohort, 59 had abdominal CT scans, 41 had abdominal ultrasounds, 16 had renal ultrasound, two had lower extremity CT angiograms, and one had an abdominal MRI scan. Of the control group of patients without the disease, 41 had ultrasound exams, 38 had abdominal CT, two had lower extremity CT angiography, and one had an MRI.
The group found that nine of patients (11%) with COVID-19 had thromboembolic findings on imaging; of these, five had medium to large arterial thrombi. Occurrence of thromboembolic findings in COVID-19 patients compared with those without the disease was statistically significant, at p = 0.02.
"Patients with solid-organ infarction had patent vasculature, suggesting the infarction may have resulted from microthrombi," the group noted.
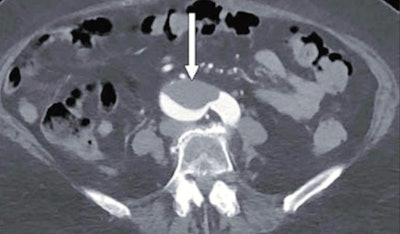 76-year-old woman who presented to emergency department with upper back pain. Axial abdominopelvic CT angiogram shows nonocclusive acute aortic thrombus (arrow). Bilateral common iliac artery and left internal iliac artery thrombi (not shown) were also seen, as well as signs of chronic atherosclerotic disease. After findings of concurrently performed chest CT raised concerns, the patient was determined to have COVID-19. Images and captions courtesy of the AJR.
76-year-old woman who presented to emergency department with upper back pain. Axial abdominopelvic CT angiogram shows nonocclusive acute aortic thrombus (arrow). Bilateral common iliac artery and left internal iliac artery thrombi (not shown) were also seen, as well as signs of chronic atherosclerotic disease. After findings of concurrently performed chest CT raised concerns, the patient was determined to have COVID-19. Images and captions courtesy of the AJR.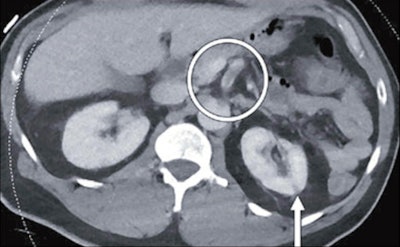 46-year-old man who was found to have COVID-19 after presenting with fever, shortness of breath, epigastric pain, and weakness. Axial contrast-enhanced abdominopelvic CT image shows small left renal infarct (arrow) and nonocclusive aortic, celiac artery, and superior mesenteric artery thrombus (circle). Complete common hepatic artery thrombus (not shown) was also seen. Splenic and renal infarctions (not shown) were present, despite patent visualized associated arteries and veins. Concurrently performed contrast-enhanced chest CT angiogram (not shown) showed lobar and segmental pulmonary emboli; probable left lower lobe pulmonary infarction rather than pneumonia; and bilateral, multilobar, patchy but confluent ground-glass opacities typical of COVID-19.
46-year-old man who was found to have COVID-19 after presenting with fever, shortness of breath, epigastric pain, and weakness. Axial contrast-enhanced abdominopelvic CT image shows small left renal infarct (arrow) and nonocclusive aortic, celiac artery, and superior mesenteric artery thrombus (circle). Complete common hepatic artery thrombus (not shown) was also seen. Splenic and renal infarctions (not shown) were present, despite patent visualized associated arteries and veins. Concurrently performed contrast-enhanced chest CT angiogram (not shown) showed lobar and segmental pulmonary emboli; probable left lower lobe pulmonary infarction rather than pneumonia; and bilateral, multilobar, patchy but confluent ground-glass opacities typical of COVID-19.The study results offer radiologists guidance when it comes to interpreting abdominal imaging results in the midst of the COVID-19 pandemic, according to Dane's team. In fact, the group pointed out that their COVID-19 patient cohort was drawn from a pool of patients who had "COVID" in their radiology report; since some patients are asymptomatic, the prevalence of the disease may be higher than what their data reflected.
"COVID-19 may present with medium to large arterial and venous abdominal and extremity macrothrombi," it concluded. "Radiologists should raise concern for COVID-19 when identifying thromboembolic abdominopelvic findings during this pandemic."