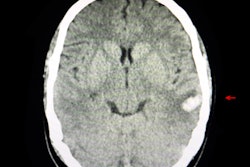
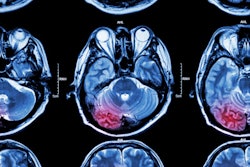
A portable low-field MRI scanner could offer an alternative to standard imaging with MRI or CT in the management of patients with suspected intracerebral hemorrhage (ICH), according to poster research presented earlier this month during the virtual annual meeting of the American Neurological Association (ANA).
Researchers from Yale University performed a research study using a portable magnet at 0.064-tesla field strength manufactured by Hyperfine Research that can be moved to the patient's bedside, said Matthew Yuen, clinical research associate of the division of neurocritical care and emergency neurology at Yale School of Medicine. Yuen presented the findings at ANA 2020.
"It has lower spatial resolution than a conventional [MRI] system, but there are instances in which point-of-care imaging may be more useful than transporting patients to a conventional radiologic suite," Yuen said. "It is another tool in our toolbox."
Yuen and co-investigators looked at images of 27 patients who had experienced ICH. They had a mean age of 61; 11 were female and 15 were white.
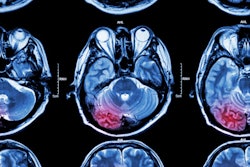
Researchers used the portable MRI scanner to obtain T2-weighted and fluid-attenuated inversion recovery (FLAIR) exams using the portable MRI system. Three raters then measured hematoma volumes on point-of-care exams and the closest standard-of-care exam (eight CT exams and 16 exams acquired within 36 hours with MRI scanners at 1.5-tesla and 3-tesla field strengths).
Point-of-care volumes were correlated against the scores calculated on the U.S. National Institutes of Health Stroke Scale (NIHSS) at the time of scan, length of hospital stay, and clinical outcome at discharge, measured by modified Rankin score.
The point-of-care MRI exams were performed within 3.4 days of symptom onset. Three patients were excluded from the analysis owing to motion degradation. Hematoma volumes ranged from 0.5 cc to 30 cc, with the median being 8.4 cc.
Yuen and co-investigators observed statistically significant intraclass coefficient correlations between point-of-care T2-weighted volumes and standard-of-care T2-weighted volumes (p < 0.01), between point-of-care FLAIR and standard-of-care FLAIR volumes (p < 0.01), and between average point-of-care (T2-weighted and FLAIR) and standard-of-care CT volumes (p < 0.01).
"We found that the portable MRI measurements were accurate compared to conventional imaging measurements," Yuen said.
Additionally, Yuen et al found point-of-care T2-weighted volumes significantly correlated with discharge clinical outcome (r = 0.55, p < 0.01), length of stay (r = 0.56, p < 0.01), and NIHSS scores at time of scan (r = 0.74, p < 0.0001). Similarly, point-of-care FLAIR volumes were significantly associated with discharge clinical outcome (r = 0.61, p < 0.01) and length of stay (r = 0.46, p < 0.05).
Yuen and co-investigators plan to enroll more patients to confirm the findings they observed in this study and to compare measurements obtained with portable MRI and standard MRI or CT at different points of time in a stroke.
Portable MRI offers several advantages, stressed Yuen.
"Portable MRI is only a fraction of the cost of conventional MRI systems," he said.
Moreover, with the need to continually clean and disinfect radiology suites during the ongoing COVID-19 pandemic, the use of portable MRI avoids transfer to the radiology suite, he pointed out.
"In a COVID-19 scenario, patients may not be getting the imaging that they need," he said, but added that even outside of the pandemic, transfer to the radiology suite carries the risk of injury.
The future of portable MRI is bright as it could serve as the great equalizer that ensures access to high-quality neuroimaging, said Yuen.
"It has incredible implications for democratizing neuroimaging to under-resourced environments," Yuen said.


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)

.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)