Functional MRI (fMRI) was helpful for evaluating persistent smell and taste dysfunction in a patient with COVID-19, according to a case report published January 22 in JAMA Neurology. The orbitofrontal cortex (OFC) appears to be particularly relevant in understanding the cause of symptoms, Kuwaiti researchers reported.
The 25-year-old female patient had been diagnosed with COVID-19, with symptoms including anosmia (loss of smell) and ageusia (loss of taste). Experience with her case was reported by Dr. Khaled Gad, PhD, and Ismail Ibrahim Ismail, both of Ibn Sina hospital in Kuwait City, Kuwait.
Although the patient was treated conservatively and started to recover, she then began to suffer from sensations of offensive odor (cacosmia) and taste (cacogeusia). Functional MRI was useful in evaluating the patient, whereas clinical exams had appeared to be normal; CT of the paranasal sinuses had been unremarkable; and no abnormalities in the olfactory bulbs and sulci were seen on brain MRI studies, the authors reported.
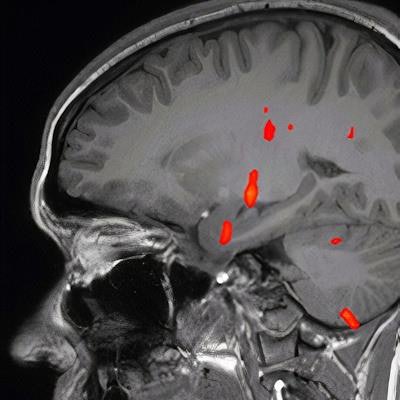
 Fused Blood oxygenation level-dependent (BOLD) map on sagittal T1-weighted image shows activation at the level of anteromedial temporal lobe, thalamus, and other regions, but absent activation of the orbitofrontal cortex. Images courtesy of Dr. Khaled Gad, PhD.
Fused Blood oxygenation level-dependent (BOLD) map on sagittal T1-weighted image shows activation at the level of anteromedial temporal lobe, thalamus, and other regions, but absent activation of the orbitofrontal cortex. Images courtesy of Dr. Khaled Gad, PhD.Problems with smell and taste are common in patients with COVID-19, occurring in an estimated 52.7% and 43.9% with the virus, respectively, according to one meta-analysis, the authors noted.
Blood oxygenation level-dependent (BOLD) activation on fMRI studies has been associated with olfactory sensation, a complex activity in the brain that involves the amygdala, the orbitofrontal cortex, and other structures, Gad and Ismail wrote.
"There is accumulating evidence of implication of OFC in patients with COVID-19 with olfactory dysfunction," they noted.
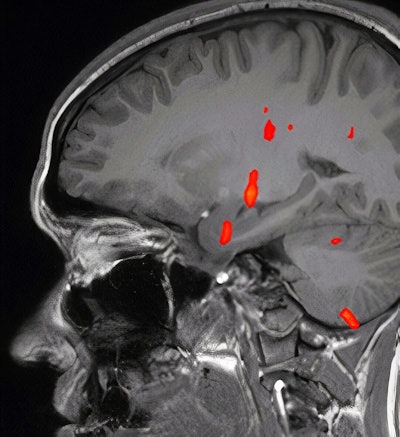
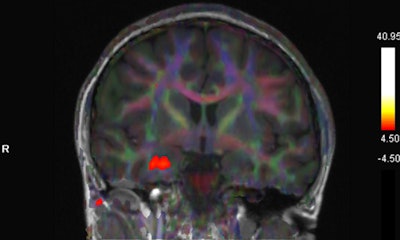 Fused BOLD and fractional anisotropy map on coronal T1-weighted image shows activation of the right uncus/piriform cortex with intact, symmetric architecture of surrounding white-matter tracts.
Fused BOLD and fractional anisotropy map on coronal T1-weighted image shows activation of the right uncus/piriform cortex with intact, symmetric architecture of surrounding white-matter tracts.The patient in the case report experienced taste and smell dysfunction for three months and had been referred to a neurology clinic, where she had a normal examination. Clinicians performed a task-based functional MRI study that involved exposure to smells and the generation of BOLD activation maps. Activation was not seen in the orbitofrontal cortex, while there was a strong BOLD signal in the right uncus/piriform cortex, they reported.
"The utility of fMRI in patients with COVID-19 is not well established, and to our knowledge this is the first published report using fMRI in a patient with persistent cacosmia and cacogeusia after COVID-19 infection," they wrote. "Given these findings, we could suggest central olfactory pathway impairment, mainly involving OFC, may be involved in the underlying etiology of persistence of olfactory and gustatory symptoms in patients after COVID-19 infection."