The use of preoperative functional MRI (fMRI) to plan brain tumor resection mitigates negative postsurgical outcomes, according to a study published June 1 in Radiology.
The research results show that fMRI offers a straightforward way to protect the long-term health of brain cancer patients, wrote a team led by Dr. Licia Luna, PhD, of Johns Hopkins Hospital in Baltimore.
"Our results suggest that preoperative functional MRI mapping results in a lower risk for delayed or permanent neurologic deficits that persist after a two-month follow-up period when compared with surgery without preoperative fMRI," the group wrote.
Although fMRI is being used more frequently as a way to better localize brain structures and tumors before brain surgery, "a considerable discrepancy between its current use and presumed utility remains," the team noted.
To address the knowledge gap, Luna and colleagues investigated overall postoperative morbidity among brain cancer patients, comparing those who underwent preoperative fMRI to those who underwent surgery without fMRI or with the use of standard neuronavigation techniques.
The study used information collected from the PubMed/Medline, Scopus, and EMBASE databases from between the years 1946 and 2020; it included 68 studies representing 3,280 participants that met any of the following criteria:
- Those evaluating patients with brain tumors
- Those evaluating patients who underwent preoperative neuroimaging workup with fMRI
- Those that investigated "the usefulness of a preoperative or intraoperative functional neuroimaging technique and used that technique to resect cerebral tumors"
- Those that reported postoperative outcomes over a two-month follow-up period
The researchers found that patients were less likely to experience negative outcomes such as neurologic, language, or motor problems after brain surgery when fMRI mapping was performed beforehand (odds ratio, 0.25) and that postsurgical Karnofsky performance status scores were higher in patients who underwent fMRI mapping (this measure ranges from zero to 100, with lower scores indicating a lower chance of a patient surviving serious illness).
The team also found that preoperative fMRI slashed the adverse event rate after brain surgery for tumor resection by almost half compared with surgery without it, at 11% compared with 21%.
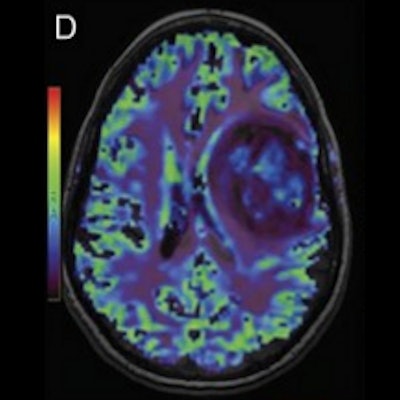
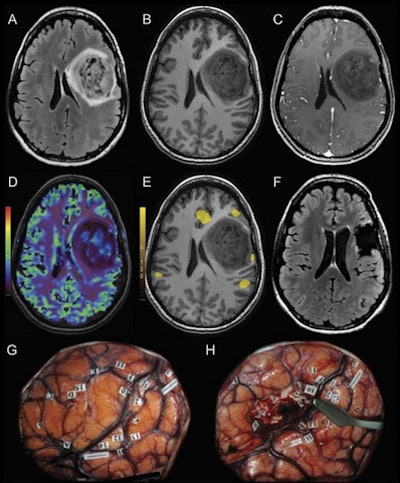 MRI scans and direct cortical stimulation technique in a 32-year-old woman with a grade II astrocytoma. Preoperative MRI shows a well-delineated mass within the left frontal lobe on (A) 3D fluid-attenuated inversion recovery (FLAIR) and (B) precontrast 3D T1-weighted scan. (C) Patchy and faint contrast enhancement is observed on postcontrast 3D T1-weighted MRI scan. (D) Cerebral blood volume map shows a globally hypoperfused tumor with hyperperfused foci. (E) Preoperative functional MRI indicates language responses surrounding the lesion. (F) Three-month postoperative FLAIR image shows complete resection of the tumor. (G) Intraoperative direct cortical stimulation helped confirm the presence of language areas (labels 10-15) in the vicinity of the tumor (demarcated by letters A-H). (H) Resection was performed according to the functional landmarks. After the surgical procedure, the patient presented with mild aphasia that completely regressed three months later. Image and caption courtesy of the RSNA.
MRI scans and direct cortical stimulation technique in a 32-year-old woman with a grade II astrocytoma. Preoperative MRI shows a well-delineated mass within the left frontal lobe on (A) 3D fluid-attenuated inversion recovery (FLAIR) and (B) precontrast 3D T1-weighted scan. (C) Patchy and faint contrast enhancement is observed on postcontrast 3D T1-weighted MRI scan. (D) Cerebral blood volume map shows a globally hypoperfused tumor with hyperperfused foci. (E) Preoperative functional MRI indicates language responses surrounding the lesion. (F) Three-month postoperative FLAIR image shows complete resection of the tumor. (G) Intraoperative direct cortical stimulation helped confirm the presence of language areas (labels 10-15) in the vicinity of the tumor (demarcated by letters A-H). (H) Resection was performed according to the functional landmarks. After the surgical procedure, the patient presented with mild aphasia that completely regressed three months later. Image and caption courtesy of the RSNA.More research is warranted, but fMRI definitely shows promise for improving brain surgery outcomes, according to the authors.
"Future studies should include clearly defined outcome measures by using objective measurements and scales and standardizing the definition of permanent neurologic deficits," they concluded. "A critical next step toward clinical acceptance of fMRI will be to develop a comprehensive set of guidelines that specifies where and when to implement fMRI in the preoperative planning of neurosurgical oncology."