Researchers are using multimodality imaging to better understand COVID-19's more unusual and long-lasting musculoskeletal effects, from rheumatoid arthritis and autoimmune myositis to redness or swelling of the feet ("COVID toes"), according to a review published February 17 in Skeletal Radiology.
X-ray, CT, ultrasound, and MRI play an important role in diagnosis and evaluation of COVID-19-related musculoskeletal pathology, wrote a team led by corresponding author Dr. Swati Deshmukh of Northwestern University Feinberg School of Medicine in Chicago.
"Advances in imaging technology have improved diagnostic capabilities for even small structures such as peripheral nerves," the group wrote. "Imaging can be utilized for initial diagnosis as well as for follow-up evaluation to assess recovery versus progression of disease ... [and in] some instances, musculoskeletal imaging may even suggest otherwise unrecognized SARS-CoV-2 infection."
Muscle soreness has been reported as a common feature of COVID-19, but other musculoskeletal conditions have begun to appear, including inflammation, nerve pain or weakness, joint diseases such as arthritis, and soft-tissue abnormalities, Deshmukh's team noted.
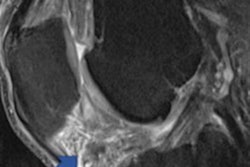
 MRI image of a patient's shoulder. The red arrow points to inflammation in the joint. The COVID-19 virus triggered rheumatoid arthritis in this patient with prolonged shoulder pain after other COVID-19 symptoms resolved. Image courtesy of Northwestern University.
MRI image of a patient's shoulder. The red arrow points to inflammation in the joint. The COVID-19 virus triggered rheumatoid arthritis in this patient with prolonged shoulder pain after other COVID-19 symptoms resolved. Image courtesy of Northwestern University."We've realized that the COVID virus can trigger the body to attack itself in different ways, which may lead to rheumatological issues that require lifelong management," Deshmukh said in a statement released by the university. "Many patients with COVID-related musculoskeletal disorders recover, but for some individuals, their symptoms become serious, are deeply concerning to the patient or impact their quality of life, which leads them to seek medical attention and imaging."
The team outlined musculoskeletal imaging findings across a range of organ systems.
| Musculoskeletal imaging findings in COVID-19 patients by body system | ||
| System | Modalities | Findings |
| Muscle | MRI, with or without contrast | Muscle swelling, necrosis, or atrophy |
| Ultrasound | Diaphragm dysfunction | |
| Nerve | MR neurography | Nerve enlargement, loss of fascicular architecture; muscle denervation |
| High resolution ultrasound | Nerve enlargement, hypoechogenicity, loss of fascicular architecture | |
| Joints | MRI with or without contrast | Joint effusion with enhancement |
| Ultrasound with Doppler | Synovitis, hyperemia | |
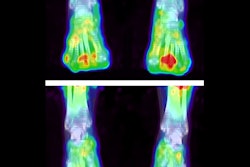
| Soft tissues | MRI, CT, ultrasound | Hematomas, gangrene, COVID toes, pressure ulcers from prone positioning |
| Bone | X-ray, CT, MRI | Osteoporosis, osteonecrosis |
Imaging helps clinicians distinguish between the virus's direct effects and ongoing conditions it may trigger, Deshmukh said in the university statement.
"If a patient has persistent shoulder pain that started after contracting COVID, their primary care provider might order an MRI/ultrasound," he said. "If a radiologist knows COVID can trigger inflammatory arthritis and imaging shows joint inflammation, then they can send a patient to a rheumatologist for evaluation."