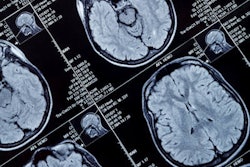
Combining clinical, electroencephalography (EEG), and MRI data better characterizes patients with neurologic effects caused by COVID-19 -- particularly COVID-19-related encephalopathy, according to a study published March 15 in JAMA Network Open.
The findings could help clinicians treat COVID-19 patients with brain injuries caused by the disease more effectively, according to a group led by Dr. Virginie Lambrecq, PhD, of the ICM Institute for Brain and Spinal Cord in Paris, France.
"The results from this cohort of patients hospitalized with COVID-19 suggest there are clinical, EEG, and MRI patterns that could delineate specific COVID-19-related encephalopathy and guide treatment strategy," the group wrote.
Brain MRI boosts diagnostic power
The SARS-CoV-2 virus can damage a patient's central nervous system, and EEG has been used to determine whether this is in the case in this population, Lambrecq's group wrote. But little research has been conducted to assess whether the benefits of EEG could be improved by adding data from imaging, particularly brain MRI.
"To our knowledge, few studies have evaluated EEG findings together with clinical, biological, and MRI findings in patients with COVID-19, and these studies did not show evidence of specific patterns," the team noted.
To address this knowledge gap, Lambrecq and colleagues conducted a study that included 78 out of 644 patients hospitalized with severe SARS-CoV-2 infection between March and June 2020 at Pitié-Salpêtrière Hospital in Paris who underwent an EEG exam. Patients were diagnosed with SARS-CoV-2 infection by either reverse transcription polymerase chain reaction (RT-PCR) assay or chest CT; they were referred to EEG for factors such as delirium, movement disorders, seizures, lack of ability to smell, or delayed awakening in the intensive care unit after sedatives were discontinued.
Of the 78 patients who had EEG, 69 showed abnormal findings such as metabolic-toxic encephalopathy features, frontal abnormalities, and epileptic activity. Of these 69, 57 underwent brain MRI; 41 were found to have irregularities. Additionally, of the 57 who underwent brain MRI, 55 were found to have biological conditions such as high sodium concentration in the blood, kidney failure, and liver dysfunction.
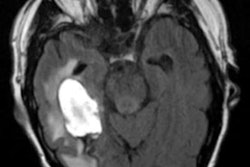
The most common abnormalities found on brain MRI in patients with neurological conditions due to COVID-19 included the following:
- Hemorrhages (21 of 57, or 37%); of these 21, 10 had multiple microhemorrhages (48%)
- Acute ischemic lesions (13 of 57, or 23%)
- Gray-matter injury (13 of 57, or 23%)
- Perfusion abnormalities (20 of 41, or 50%); of patients with perfusion abnormalities, 95% had hypoperfusion
The group developed a regression model that could identify patients with COVID-19-induced encephalopathy that included data from periodic EEG discharges, movement disorders, brainstem impairment, frontal syndrome, and white matter-enhancing lesions on MRI. The model showed the following performance for estimating the risk of COVID-19-related encephalopathy:
| Performance of risk model for estimating patients COVID-19-induced encephalopathy risk | |
| Measure | Model performance |
| Accuracy | 91% |
| Negative predictive value | 95% |
| Positive predictive value | 65% |
| Sensitivity | 76% |
| Specificity | 93% |
"In our study, we showed that patients with COVID-19-related encephalopathy mostly had movement disorders (mainly seizures and/or myorrhythmia), and brainstem impairment (oculomotor disorders such as bobbing) and frontal syndrome (disinhibition and grasping)," the group wrote. "Similarly, MRI findings showed both ... unspecific lesions, such as perfusion abnormalities, and ... more specific lesions, such as basal ganglia abnormalities, microhemorrhages, corpus callosum injury, and white matter-enhancing lesions."
More data = better diagnosis
Combining clinical, EEG, and MRI data appears to improve diagnosis of neurological conditions associated with COVID-19, according to the researchers.
"Despite different clinical presentations, our study suggests that EEG is a valuable procedure for patients with COVID-19 and neurologic symptoms, to better identify different brain dysfunctions and COVID-19-related encephalopathy," they concluded. "We further emphasize the benefit associated with combining EEG and brain MRI for patients with neurologic symptoms concomitant with COVID-19. It remains to be clarified whether treatment strategies could be optimized with earlier identification of patients with COVID-19-related encephalopathy."