MRI reveals brain changes in adults with herpes simplex encephalitis (HSE) that are associated with poorer neurological outcomes at 90 days after admission to the intensive care unit (ICU), according to a study published July 27 in JAMA Network Open.
These changes often manifest as thalamic diffusion signal variations, and awareness of them could help clinicians manage HSE patients better, wrote a team led by Dr. Benjamine Sarton of the University Hospital of Purpan in Toulouse, France.
"The poor outcome that we report emphasizes the importance of further research to design and validate more personalized intervention strategies for these patients, which will be at least in part built upon brain MRI data," the team wrote.
HSE is the most common cause of sporadic necrotizing encephalitis around the world, and if untreated, it has a mortality rate of roughly 70%, the authors noted. Although methods of diagnosis have improved -- and acyclovir treatment has reduced the mortality rate to 15% -- many of those who contract the disease remain disabled. That's why using MRI to help predict outcomes is so promising, according to Sarton and colleagues.
"The identification of early and reliable indicators of outcomes in patients with severe HSE might constitute a game-changing factor, leading to more personalized intervention strategies," the team wrote. "MRI enables fast diagnosis and permits disentangling of HSE from its mimics."
However, there are few studies investigating the prognostic value of brain MRI with HSE. To address the knowledge gap, Sarton's group conducted a study that explored associations between MRI findings and HSE patients' functional outcomes at 90 days after admission to the ICU.
The research included 138 patients diagnosed with encephalitis who tested positive for herpes simplex virus in their cerebrospinal fluid between 2007 to 2019 at 34 ICUs in France. The patients underwent a standard brain MRI exam within 30 days of admission; for the study, these exam findings were analyzed by radiologist readers blinded to patient outcomes. Poor outcomes at 90 days after ICU admission were scored on a scale of three to six (moderate-to-severe disability or death).
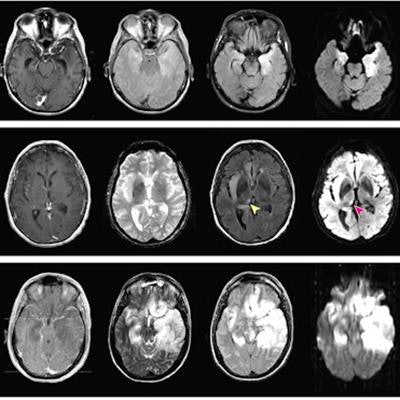
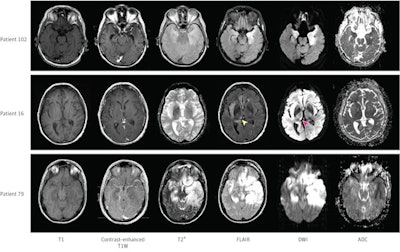 Patient 102 had bilateral but asymmetrical hyperintensities in the temporal lobes seen on fluid-attenuated inversion recovery (FLAIR) images and diffusion-weighted imaging (DWI) magnetic resonance imaging sequences. Patient 16 had right thalamic hypersignal on FLAIR and DWI sequences (arrowheads), ipsilateral to the insular lesion. Patient 79 had extensive brain lesions, showing bilateral temporal, frontal, and insular signal abnormalities. ADC indicates apparent diffusion coefficient; T1W, T1-weighted. Image and caption courtesy of JAMA Network Open.
Patient 102 had bilateral but asymmetrical hyperintensities in the temporal lobes seen on fluid-attenuated inversion recovery (FLAIR) images and diffusion-weighted imaging (DWI) magnetic resonance imaging sequences. Patient 16 had right thalamic hypersignal on FLAIR and DWI sequences (arrowheads), ipsilateral to the insular lesion. Patient 79 had extensive brain lesions, showing bilateral temporal, frontal, and insular signal abnormalities. ADC indicates apparent diffusion coefficient; T1W, T1-weighted. Image and caption courtesy of JAMA Network Open.Sarton's team found that, at 90 days post-ICU admission, 95 patients (68.8%) had a poor outcome, including 16 deaths (11.6%). The group also found that there were particular factors associated with these outcomes.
| Factors associated with poor functional outcome in HSE patients admitted to the ICU | |
| Factor | Odds ratio |
| More than three lobes involved on fluid-attenuated inversion recovery sequence | 25.71 |
| Age 60 or older | 7.62 |
| Hypersignal in left thalamus | 6.90 |
| Simplified acute physiology score of more than 34 | 3.91 |
| Bilateral lesions on diffusion-weighted imaging sequence | 3.17 |
"We observed that the total amount of neuroinflammatory lesions, which were mainly identified by FLAIR [fluid-attenuated inversion recovery] acquisitions, was significantly associated with patients' functional outcomes," the group wrote.
More research is definitely needed, according to Sarton's team.
"In this cohort study of patients with HSE, the presence of extensive MRI lesions, on both FLAIR and [diffusion-weighted imaging (DWI)] sequences, was independently associated with poor functional outcome at 90 days," the group wrote. "Thalamic DWI hyperintensities were frequently observed and were associated with poor prognosis, mainly in older patients. Future studies should focus on prospectively testing the prognostic value of these neuroimaging markers."