Breast MRI shows that intrauterine contraceptive devices (IUDs) have systemic effects on the body and not just the uterus. The phenomenon could affect the accuracy of breast MRI, according to research being presented at the RSNA 2021 annual meeting.
A team led by Dr. Luisa Huck from Aachen University in Germany found that IUDs can lead to increased background parenchymal enhancement (BPE). The researchers said these findings counter claims that the effects of IUDs are limited to the uterus.
"Moreover, the observed increased BPE supports the observation that IUDs can lead to side effects similar to hormone replacement therapy," Huck and colleagues wrote.
Levonorgestrel-releasing IUDs are widely used by women worldwide for birth control. They release a small amount of hormone directly into the uterus, meaning the amount of hormone in the bloodstream is lower than with other hormonal methods.
Previous claims have said that any side effects of the IUDs are confined to the uterus due to the limited area of release. However, recent research suggests that IUDs can be associated with side effects similar to those of systemic hormonal medication in other parts of the body.
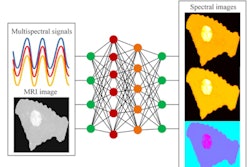
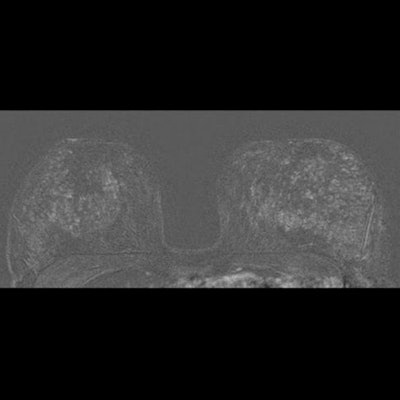
Background parenchymal enhancement is the initial enhancement of normal breast tissue, which also serves as a sensitive marker of hormone levels. Researchers at Aachen University said they noticed that women with a hormonal IUD in place often show higher BPE on contrast-enhanced breast MRI.
Huck et al wanted to study the link between IUD use and BPE in breast MRI and look at the possible systemic effects of IUDs.
They looked at the university hospital's database and included 48 premenopausal women with an average age of 45 years who did not have a personal history of breast cancer or hormone or antihormone intake. They also had undergone standardized dynamic contrast-enhanced breast MRI for screening at least twice between 2014 and 2020.
Half of the women in the study underwent the first breast MRI exam before IUD placement and the second with the IUD in place. The other half had their first MRI with IUD placement and the second MRI after IUD removal, with a minimum time of four weeks after placement or removal.
"To avoid confounding ageing-related effects on BPE, half of included women had to have their first MRI without, the other half had their first study with IUD in place," they added.
Degree of BPE was analyzed according to categories set by the American College of Radiology (ACR).
In 24 of the women, ACR categories did not change with versus without an IUD. However, researchers found that IUD use led to significant increase of enhancement in 23 patients, suggesting that there are hormonal effects caused by IUD use that occur well beyond the uterus. One patient had an ACR category lower with versus without an IUD.
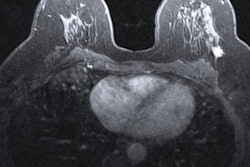
 Breast MRI of a 41-year-old patient. The left image is without an IUD in place, while the right image shows increased parenchymal enhancement in the same patient 27 months after IUD placement.
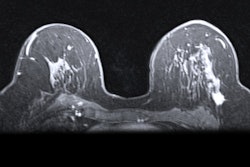
Breast MRI of a 41-year-old patient. The left image is without an IUD in place, while the right image shows increased parenchymal enhancement in the same patient 27 months after IUD placement. Breast MRI of a 45-year-old patient. The left image is with an IUD in place, while the right image is from the same patient 32 months after IUD removal.
Breast MRI of a 45-year-old patient. The left image is with an IUD in place, while the right image is from the same patient 32 months after IUD removal.The researchers said that the change of ACR category depending on presence or absence of an IUD was statistically significant (p < 0.001).
"Radiologists should be aware that women with an IUD have a higher BPE. Therefore, precancerous lesions may be more difficult to diagnose," Huck told AuntMinnie.com.
Despite the effects, Huck said that IUDs appear to be a safe, tolerable contraceptive. However, she added that women who have unexplainable side effects should consult with their physicians on other types of contraception.