Nonscanning time between abbreviated breast MRI exams contributes to workflow problems, preventing more patients from being imaged, according to research presented Sunday at the RSNA 2021 annual meeting.
In his presentation, Dr. Philipp Stelzer from the Medical University of Vienna said that clinical practice improvements should focus on this organizational problem rather than not including diagnostically useful image acquisition.
"Protocol abbreviation does not proportionally translate into total exam time reduction," Stelzer said. "We have to take nonscanning time parameters into consideration ... we should prioritize to reduce this parameter first."
MR mammography is the most sensitive test for breast cancer detection, the researchers said. Imaging protocols are increasingly abbreviated to increase the number of patients imaged per day, which saves table time.
Researchers have not reached a consensus on what "abbreviated" MR mammography is and approaches vary. However, the number of patients that can be examined per MRI unit each time also depends on the table switching time between patients.
Stelzer et al wanted to collect breast MRI measurement times in different clinical scenarios.
"We wanted to see how nonscan time comes into play," Stelzer said.
The team retrospectively looked at data from four study sites, including tertiary care centers and outpatient centers, and examined protocols from each. A total of 79 breast MRI examinations were evaluated.
 Researchers from Austria found that nonscanning parameters affect workflows on abbreviated breast MRIs. They compared exam ratios when nonscanning parameters are included and excluded in imaging protocols. Image courtesy of Dr. Philipp Stelzer.
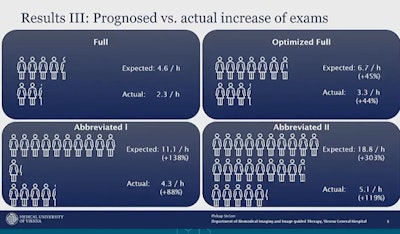
Researchers from Austria found that nonscanning parameters affect workflows on abbreviated breast MRIs. They compared exam ratios when nonscanning parameters are included and excluded in imaging protocols. Image courtesy of Dr. Philipp Stelzer.The group found that abbreviated examination protocols lead to a much smaller number of screenings than expected. Stelzer and colleagues calculated the number of exams possible if nonscanning parameters were included.
For a full protocol, radiologists could be expected to perform 4.6 exams per hour. However, with the nonscanning parameters, they could only perform 2.3 per hour.
"For the shortest protocol so far with a three-minute scan time, we should be able to do 18.8 exams per hour for which there would be no nonscanning time," Stelzer said. "But actually, we are only able to do 5.1 per hour if we include nonscanning time parameters."
Stelzer also said about 74% of time spent with an imaging protocol is dedicated toward nondiagnostic activities, including table switching and planning.
The researchers also found that the median table time was significantly shorter in the outpatient setting, at 10.2 minutes, compared with the 13.3 minutes seen at tertiary care centers (p < 0.001).
However, they also found no significant differences in median table switching time between the tertiary care center and outpatient centers. Switching-imaging ratio and relative switching time were also significantly lower in the tertiary care setting.
Stelzer said two things to keep in mind when looking at imaging protocols for abbreviated breast MRI are that scanning time equals potential diagnosis information while nonscanning time has no diagnostic benefit.
With that said, Stelzer also noted that clinics can implement practices such as admitting patients early and providing them with multiple imaging preparation rooms for better throughput.