Radiologists must be aware that metallic markers are responsible for artifacts in breast MRI exams, according to Swiss researchers. These artifacts can be of different types and sizes, depending on the MRI sequence, magnetic field, and marker type, they say.
"Knowledge of these artifacts improves the quality of the interpretation," Dr. Matthias Hugot, chef de clinique in the department of medical imaging at the Réseau hospitalier neuchâtelois in Neuchâtel, Switzerland, told AuntMinnieEurope.com on August 3.
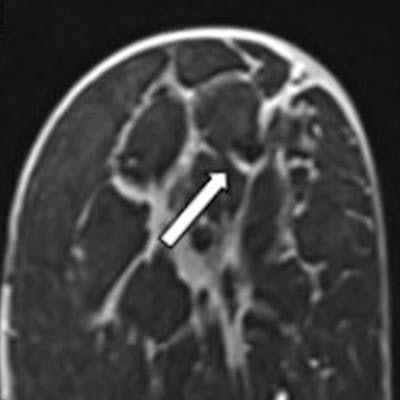
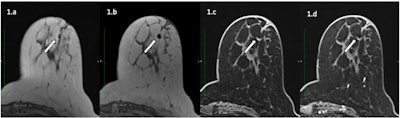 A 57-year-old patient with an invasive ductal carcinoma marked by an O-Twist metallic marker and treated with neoadjuvant chemotherapy underwent a presurgical MRI on a Siemens 3T with T2-weighted (a), T1-weighted (b), and 3D T1-weighted Dixon before (c) and after (d) contrast injection. Metallic marker is responsible for a hyposignal artifact with hyperintense peripheral halo. However, diagnostic confidence was 3 for both readers. Despite the relatively small size of the artifact, the small initial size of the tumor (7 mm) resulted in uncertainty in appreciations of both readers in the presence of the metallic marker artifact. The patient was considered rCR but histology revealed the presence of residual tumor. All figures courtesy of Dr. Matthias Hugot et al and European Journal of Radiology.
A 57-year-old patient with an invasive ductal carcinoma marked by an O-Twist metallic marker and treated with neoadjuvant chemotherapy underwent a presurgical MRI on a Siemens 3T with T2-weighted (a), T1-weighted (b), and 3D T1-weighted Dixon before (c) and after (d) contrast injection. Metallic marker is responsible for a hyposignal artifact with hyperintense peripheral halo. However, diagnostic confidence was 3 for both readers. Despite the relatively small size of the artifact, the small initial size of the tumor (7 mm) resulted in uncertainty in appreciations of both readers in the presence of the metallic marker artifact. The patient was considered rCR but histology revealed the presence of residual tumor. All figures courtesy of Dr. Matthias Hugot et al and European Journal of Radiology.Hugot and his colleagues from Geneva University Hospital have just published the findings of a study on this topic. The results, published on July 28 in the European Journal of Radiology, show that the diagnostic performance of preoperative MRI after neoadjuvant chemotherapy (NAC) for the prediction of Pathological Complete Response (pCR) did not differ statistically in the presence or absence of metallic markers.
"Diagnostic performance for detecting pCR to NAC was the same regardless of the presence of a marker," they noted. "The type of metallic marker, between the two major categories studied, did not influence diagnostic performance of readers for detecting pCR. Interreader agreement was high regardless of the presence of a marker."
Study details
The researchers included all consecutive patients who underwent preoperative breast MRI after completion of NAC (mean, 4.4 days +/- 15.9). They recorded the presence or absence of markers, the type of markers, and the size and type of artifact on each MRI sequence.
Two radiologists who were blinded to histopathological results and to each other's findings evaluated all MRI exams for the presence or absence of complete response. Pathology was the standard of reference. Diagnostic performance of MRI for the prediction of pCR in the presence or absence of markers -- and also between the two most popular brands of marker (O-Twist and UltraClip) -- was compared using Chi-squared tests or equivalents.
Ninety-three patients (mean age, 48 +/- 11) were included in the Swiss study. Nineteen of them had no markers and 74 had 108 markers. Sensitivity and specificity of MRI for the prediction of pCR were 0.73 and 0.81 for patients with and 0.67 and 0.90 for patients without markers (p < 0.05), respectively. There was no statistical difference in the performance of MRI for the two different types of markers studied.
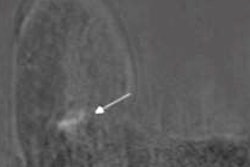
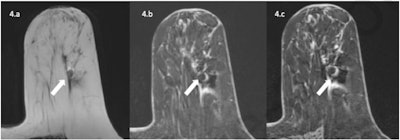 A 63-year-old patient with invasive ductal carcinoma marked by an Ultraclip metallic marker and treated with neoadjuvant chemotherapy underwent a preoperative 1.5T MRI exam with T2-weighted, 3D T1-weighted VIBE before and after contrast media injection. Metallic marker is responsible for a hypointense artifact with hyperintense halo more important with fat saturation than Dixon sequences as expected. Because of this artifact, the patient was considered Radiological Complete Response (rCR) with low diagnostic confidence from both readers, but residual tumor was detected in final pathology results.
A 63-year-old patient with invasive ductal carcinoma marked by an Ultraclip metallic marker and treated with neoadjuvant chemotherapy underwent a preoperative 1.5T MRI exam with T2-weighted, 3D T1-weighted VIBE before and after contrast media injection. Metallic marker is responsible for a hypointense artifact with hyperintense halo more important with fat saturation than Dixon sequences as expected. Because of this artifact, the patient was considered Radiological Complete Response (rCR) with low diagnostic confidence from both readers, but residual tumor was detected in final pathology results.The authors' hope was that the clips were not responsible for a decrease in the diagnostic accuracy of MRI, which would have called into question the interpretation of post-NAC breast MRI, Hugot explained.
"The most surprising result was to see that diagnostic confidence is impacted by the presence of the clip -- without, however, impacting diagnostic accuracy," he noted.
Hugot admitted that there are several limitations of the study due to the retrospective nature of the research and the small number of patients in the study population. Because of these, he believes it is essential to conduct further research on a larger scale so that it becomes possible to generalize the group's results. He also thinks it's important to test more clips from other manufacturers.
Overall, the Swiss authors report that magnetic markers are widely visible on MRI images due to the susceptibility artifact that they generate.
"However, the same artifact that accounts for visibility of the marker can possibly mask or mimic, depending on the circumstances, a residual tumoral enhancement and thus reduce the diagnostic accuracy of MRI," they wrote. "Indeed, the size and appearance of metallic artifact on MRI depends on several factors, namely the material of the clip (in particular its magnetic susceptibility), the magnetic field strength of the system, and the sequence itself (gradient echo or spin echo are not equally sensitive to the presence of metal)."