MRI visualizes features in breast tissue in women who have been treated for the disease that are associated with risk of second breast cancer, a study published August 30 in Radiology indicates.
Specifically, the ability to assess the level of background parenchymal enhancement (BPE) on surveillance MRI could help tailor breast cancer treatment follow-up, noted a team led by Dr. Su Hyun Lee, PhD, of Seoul National University Hospital.
"Information obtained with BPE may help to better define the risk of second breast cancer and tailor imaging surveillance strategies," the group wrote. "For example, women with minimal BPE at surveillance breast MRI may no longer need to undergo contrast-enhanced breast MRI every year."
Breast cancer is the leading cause of cancer-related death in women around the world. Mammography is the gold standard for breast cancer screening, but it is less effective in women with dense tissue due to its 2D nature. Women with dense breasts often undergo supplemental screening, and breast MRI is one of the most effective tools.
But even after diagnosis and treatment via surgery, some women are vulnerable to breast cancer recurrence, Lee and colleagues explained. So they sought to investigate any connection between second breast cancer risk and breast tissue density as visualized as background parenchymal enhancement on contrast-enhanced MRI.
To do so, the investigators conducted a study that included 2,668 women who underwent surveillance breast MRI scans between January 2008 and December 2017 after surgery for primary breast cancer. Of these, 109 presented with a second breast cancer at median follow-up of six years.
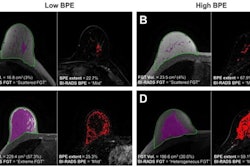
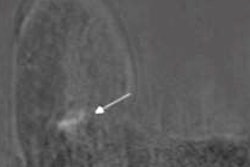
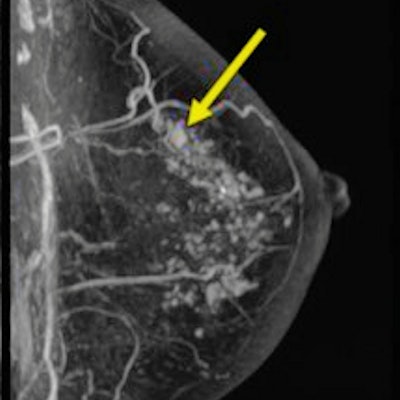
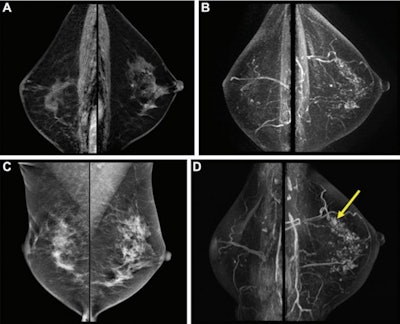 Postoperative surveillance images in a 54-year-old woman who had undergone right breast-conserving surgery and postoperative radiation therapy two years prior for stage III hormone receptor-positive invasive ductal carcinoma. She had completed adjuvant chemotherapy and was on endocrine therapy. She had no family history of breast cancer and had not been tested for the BRCA1/BRCA2 genes. (A) Bilateral sagittal contrast-enhanced T1-weighted and (B) maximum intensity projection images from baseline surveillance breast MRI show asymmetric moderate background parenchymal enhancement in the left breast. (C) Surveillance mammograms acquired within six months of surveillance breast MRI show heterogeneously dense breasts. (D) Subsequent surveillance breast MRI scans acquired two years after baseline surveillance breast MRI show a small irregular enhancing mass in the left upper breast (arrow). Biopsy and surgical pathologic examination revealed a 0.8-cm ductal carcinoma in situ.
Postoperative surveillance images in a 54-year-old woman who had undergone right breast-conserving surgery and postoperative radiation therapy two years prior for stage III hormone receptor-positive invasive ductal carcinoma. She had completed adjuvant chemotherapy and was on endocrine therapy. She had no family history of breast cancer and had not been tested for the BRCA1/BRCA2 genes. (A) Bilateral sagittal contrast-enhanced T1-weighted and (B) maximum intensity projection images from baseline surveillance breast MRI show asymmetric moderate background parenchymal enhancement in the left breast. (C) Surveillance mammograms acquired within six months of surveillance breast MRI show heterogeneously dense breasts. (D) Subsequent surveillance breast MRI scans acquired two years after baseline surveillance breast MRI show a small irregular enhancing mass in the left upper breast (arrow). Biopsy and surgical pathologic examination revealed a 0.8-cm ductal carcinoma in situ.The researchers found that the presence of "mild, moderate, or marked" BPE on surveillance breast MRI was associated with an increased risk of future second breast cancer compared with minimal BPE. There were other factors as well: In fact, positive BRCA1/BRCA2 genetic test results increased the risk of second breast cancer by over sixfold, and being younger than 45 at time of initial cancer diagnosis increased risk by more than threefold.
| Factors contributing to higher risk of second breast cancer after diagnosis and surgical treatment of primary breast cancer | |
| Factor | Hazard ratio* |
| Positive BRCA1/ BRCA2 genetic test results | 6.5 |
| Younger than 45 years of age at initial breast cancer diagnosis | 3.4 |
| Mild, moderate, or marked BPE at surveillance MRI | 2.1 |
| Negative hormone receptor expression in initial breast cancer | 1.6 |
*1 is reference; higher values equal greater risk.
The study results could help tailor follow-up of women who have been treated for breast cancer, Lee said in the RSNA statement.
"Our study results may help to stratify the risk of second breast cancer in women with a personal history of breast cancer and to establish personalized imaging surveillance strategies in terms of imaging modality and monitoring interval selection," she said. "For example, women with minimal BPE at surveillance breast MRI may no longer need to undergo contrast-enhanced breast MRI every year if other risk factors are absent."
Many questions remain about how to incorporate BPE information into ongoing care for women who have been treated for primary breast cancer, noted Dr. Bethany Niell, PhD, of the University of South Florida in Tampa, in a commentary that accompanied the study.
"Although many questions remain unanswered, the results from the study by Lee et al provide additional impetus for future avenues of research into the clinical and biologic implications of BPE at breast MRI," she wrote.