While MRI-detected biomarkers may serve a beneficial role for people with hip and knee pain, the modality's clinical utility may be limited in patients over the age of 45 with advanced osteoarthritis, according to an article published in the American Journal of Roentgenology (AJR).
After performing a systematic review and meta-analysis of current literature to assess the clinical utility of MRI in this patient population, NYU Langone Health researchers found several knee structural lesions on MRI that represented potential imaging biomarkers. However, they also found that identifying meniscal tears on MRI likely has diminished clinical value.
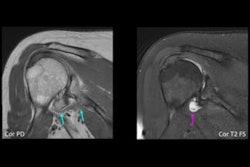
"For the hip, MRI can play a role in the diagnosis of labral tears, chondral lesions, and femoroacetabular impingement in patients without advanced osteoarthritis," the authors wrote.
 Erin Alaia, MD.
Erin Alaia, MD.
Although pathology on MRI correlating with symptoms guides clinical decision-making in younger patients, osteoarthritis and coexistent pathology such as meniscal or labral tears are increasingly evident with advancing age, according to Erin Alaia, MD, Mohammad Samim, MD, and colleagues from NYU Langone Health's department of radiology with collaborators from NYU Langone Health's department of orthopedic surgery and the University at Buffalo Jacobs School of Medicine and Biomedical Sciences.
"There is an increased awareness and discussion around the appropriateness of imaging the middle-aged and older patient population," Alaia explained for AuntMinnie.com. "We believe that patients should not be excluded from advanced imaging based on age alone. MRI can play a useful role in treatment decisions for these patient populations, such as arthroscopic intervention or steroid injection, when important factors like osteoarthritis are considered."
The utility of advanced imaging with MRI in middle-aged and older patients has been called into question, particularly in the setting of osteoarthritis, Alaia and colleagues noted. For example, "in the presence of osteoarthritis, MRI-diagnosed intraarticular pathology such as meniscal tears does not always correlate with symptoms, and may not benefit from arthroscopic surgery."
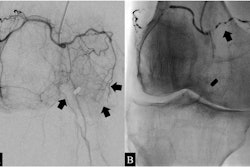
To assess evidence of MRI's clinical value in knee imaging, radiologists who had been practicing for 11 to 13 years reviewed 18 knee studies (10 prospective and 8 retrospective) published between 2001 and 2020, involving 5,907 patients from 45 to 90 years old. Studies included ranged from bone only to both bone and soft tissues and only soft tissues. Reviewers also looked at the correlation of soft-tissue pathology with symptoms.
Commenting on the impact of surgery on meniscal tears for those with mild to moderate osteoarthritis, for example, Alaia and colleagues noted that at six months there was no difference in functional improvement between the surgical and physical therapy groups.
"Bone marrow edema-like lesions, joint effusions, and synovitis on MRI were associated with symptoms," the authors wrote. "In patients with osteoarthritis, meniscal tears were less likely to be symptom generators and were less likely to respond to arthroscopic surgery with osteoarthritis progression."
For evidence of MRI's clinical value in hip imaging, reviewers evaluated 13 studies (11 retrospective and two prospective) published in orthopedic surgery journals between 2015 and 2021, involving 6,385 patients from 50 years old to over 85. For MRI of the hip, Alaia and colleagues concluded that MRI can add value in certain applications.
"Patients with Tonnis grade 2 osteoarthritis and lower with and without femoroacetabular impingement showed improved outcomes after arthroscopy, suggesting a role for MRI in the diagnosis of labral tears, chondral lesions, and femoroacetabular impingement," the authors wrote. "Although this group benefited from arthroscopic surgery, outcomes were inferior to those in younger patients."
Moreover, MRI biomarkers are used in clinical trials to monitor the appropriateness of initiating therapy and monitoring treatment response, Alaia told AuntMinnie.com. "Since these MRI biomarkers have been found to correspond to pain (i.e., bone marrow edema-like lesions, or synovitis), they suggest a usefulness of MRI even in patients with known osteoarthritis as these imaging findings can help determine if a patient would be a candidate for therapy (i.e., viscosupplementation, steroid injection), and possibly assist with monitoring treatment response."
From 1,125 potential studies identified through PubMed, Web of Science, and Embase through October 3, 2022, only the 31 explained in the AJR article met the criteria for inclusion in this systematic review and meta-analysis. Study methods were appraised via NIH Quality Assessment Tools.
"The most important take-home point of this manuscript is that when we think about imaging and possible surgical management for middle-aged and older patients, we should not make assumptions about the appropriateness of imaging or therapies based on patient age alone," Alaia said.
Read the full review here.