The use of breast MRI has increased 14-fold since the American College of Radiology (ACR) changed its guidelines in 2018, a study presented May 7 at the American Roentgen Ray Society (ARRS) annual meeting found.
In her talk, Madeline Floodstrand from Rush University Medical Center in Chicago, IL, discussed her team’s findings, which also showed that breast density had the largest impact on MRI uptake of any single risk qualification for women with a personal history of breast cancer. Also, women with both dense breasts and a known genetic mutation had the largest MRI uptake of any risk cohort.
“These findings, we believe, are attributable to increased social awareness and patient education surrounding the challenges of cancer detection with breast density,” Floodstrand said.
The ACR’s 2018 guideline changes impacted MRI screening for women with a personal history of breast cancer. Previously, only women with a personal history of breast cancer and a known genetic mutation were recommended for annual screening MRI in addition to mammography. The current guidelines recommend women with a personal history of the disease and who have dense breasts or cancer diagnosis before age 50 for supplemental breast MRI.
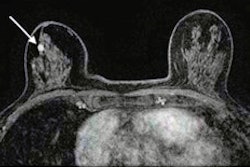
Floodstrand and colleagues hypothesized that this expansion is expected to have a positive impact on breast health, highlighting MRI’s high sensitivity in detecting breast cancer. The team evaluated the extent of these new guidelines’ impact on eligibility for supplemental screening. It also explored differentiating factors that may impact MRI use in this population.
The study included data from 929 women, of which 664 had dense breasts and 541 were diagnosed with breast cancer at younger than 50 years old. Also, 65 women had a known genetic mutation, representing those who qualified for MRI before the 2018 guideline changes.
The team reported that 325 of the women received the recommended supplemental MRI, while 604 did not. From the total study population, the researchers reported a cancer detection rate of 18.3, with 88.3% being minimal cancers under 10 mm in size.
After the ACR guideline changes, Rush's patient population that is eligible for supplemental screening with MRI increased by nearly 14-fold (1,329.23%).
The following factors showed significant differences in MRI uptake:
Increasing age was tied to decreasing MRI uptake (p < 0.0001).
Patients with high-risk providers had higher uptake of MRI (p = 0.004).
Patients with commercial insurance had higher MRI uptake than those with Medicare/Managed Care (p = 0.0034).
Breast density meanwhile has a significant role in MRI uptake, the researchers found. This includes breast density being the only risk category in the study with significantly higher MRI uptake (p < 0.0001).
Also, women with dense breasts alone had higher MRI uptake than those only with diagnosis under age 50 (p = 0.0153), and women with dense breasts and diagnosis under age 50 had higher uptake than those with only diagnosis under this age (p < 0.0001). Additionally, women with dense breasts and a known genetic mutation had significantly higher MRI uptake than those with only diagnosis under age 50 (p = 0.0379).
Finally, the team reported no significant differences in MRI uptake regarding race or language.
Floodstrand said that the results indicate that MRI does its job in detecting cancers early in this population. She added that 100% of the cancers found in the study population were node-negative and 100% were stage 0 or 1.
“It’s important to talk about this [breast density] because it’s really common,” Floodstrand said. “Somewhere between 43% and 46% of women over the age of 40 have been found to have dense breasts.”