Time-dependent diffusion MRI-based microstructural mapping helps predict breast cancer molecular subtypes and treatment response in women with the disease, researchers have reported.
A team led by Xiaoxia Wang of Chongqing University Cancer Hospital in China found that the technique outperformed apparent diffusion coefficient (ADC) measurements and a clinical-pathologic model when it came to predicting treatment response, with an area under the receiver operating curve (AUC) of 0.88 compared with 0.73 (ADC) and 0.79 (clinical-pathologic model).
"[Our study showed that] time-dependent diffusion MRI–based microstructural mapping [is] an effective method in helping to identify molecular subtypes and predict pathologic complete response to neoadjuvant chemotherapy in participants with breast cancer," the group wrote.
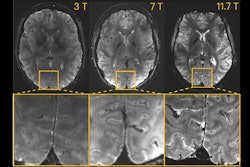
Time-dependent diffusion MRI is a technique that uses diffusion MRI signals acquired at various diffusion times to characterize tissue microstructures, the team explained. It has the potential to characterize tumor cell properties but hasn't been evaluated for breast cancer diagnosis and treatment response prediction.
To this end, the investigators conducted a study that investigated whether time-dependent diffusion MRI-based microstructural mapping could work for these indications. The research included 408 women with breast cancer who underwent a time-dependent diffusion MRI exam between February 2021 and May 2023. They also evaluated the women with three apparent diffusion coefficient (ADC) measurements and a relative ADC diffusion-weighted imaging parameter. They then created a predictive model and assessed its performance using the area under the receiver operating curve (AUC) measure.
Of the 408 study participants, 221 underwent neoadjuvant chemotherapy. Of these, 54 (24.4%) showed positive treatment response.
The group found the following:
- Time-dependent diffusion MRI parameters showed reasonable performance in helping to identify luminal A (AUC, 0.7), luminal B (AUC, 0.78), and triple-negative breast cancer (AUC, 0.72) breast cancer subtypes and high performance for human epidermal growth factor receptor 2 (HER2)-enriched breast cancer (AUC, 0.85), outperforming ADC measurements.
- Progesterone receptor status, HER2 status, and the cellularity index were independently associated with the odds of achieving positive treatment response (odds ratios, 0.08, 3.36, and 0.01, respectively).
- The model demonstrated high performance for predicting positive treatment response, outperforming ADC measurements and the clinical-pathologic model with an AUC of 0.88 compared to 0.73 and 0.79, respectively.
- Time-dependent diffusion MRI-estimated parameters correlated well with pathologic measurements (Pearson correlation measure 0.67 to 0.81, with 1 as reference; p < 0.001).
"In our study, time-dependent diffusion MRI microstructural parameters demonstrated excellent performance in helping to identify four molecular subtypes … which was better than that of the apparent diffusion coefficient parameters derived from diffusion-weighted imaging," the authors concluded.
The complete study can be found here.