Contrast-enhanced mammography (CEM)-guided biopsy by itself is not a good substitute for MRI-guided biopsy of suspicious breast MRI findings, according to a study published September 18 in the American Journal of Roentgenology.
Researchers led by Michael Morris, MD, from Banner MD Anderson Cancer Center in Gilbert, AZ, reported that more than one-quarter of suspicious MRI findings deemed to be occult at attempted CEM-guided biopsy were diagnosed as malignant by subsequent MRI-guided biopsy.
“In the current state, CEM-guided biopsy should not be extended to the biopsy of suspicious findings on MRI,” Morris told AuntMinnie.com.
MRI-guided breast biopsy is effective for the workup of suspicious MRI findings. However, the researchers noted that it is a time-consuming and resource-intensive procedure. Recent research has highlighted the potential of CEM as a substitute for MRI in diagnostic imaging in terms of imaging accuracy and patient accessibility, and the technique has been explored as an alternative sampling method for enhancing lesions.
Morris and colleagues evaluated their institution's experience in performing initial attempted CEM-guided biopsy for suspicious breast MRI findings.
The study included data collected in 2023 and 2024 from 155 women who underwent breast MRI assessed as BI-RADS 4 or 5. Of the total cohort, 73 received the option for attempted CEM-guided biopsy, with 21 undergoing it. Two breast radiologists with 12 and 13 years of post-training experience independently reviewed images from completed CEM-guided and MRI-guided biopsies.
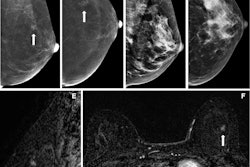
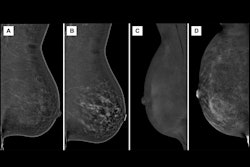
 (A, B) Images depict a 65-year-old woman with prior left malignant lumpectomy. (A) Sagittal fat-suppressed contrast-enhanced T1-weighted image from diagnostic MRI performed for clear left nipple discharge shows segmental nonmass enhancement (NME) (arrows), deemed suspicious with assessment as BI-RADS category 4. The patient elected to undergo attempted contrast-enhanced mammography (CEM)-guided biopsy rather than direct MRI-guided biopsy. (B) Recombined scout image from attempted CEM-guided biopsy shows corresponding NME (arrows), serving as the biopsy target. CEM-guided biopsy was completed. Histologic assessment yielded benign findings, deemed concordant by the performing radiologist. (C,D) Images depict a 55-year-old woman with left breast invasive ductal carcinoma (IDC). (C) Sagittal fat-suppressed contrast-enhanced T1-weighted MR image from staging MRI shows known IDC (arrowhead) and additional 4-mm NME (arrow), deemed suspicious with assessment as BI-RADS category 4. Only NME was considered to represent a suspicious finding warranting biopsy. The patient elected to undergo attempted CEM-guided biopsy rather than direct MRI-guided biopsy. (D) Recombined scout image from attempted CEM-guided biopsy shows an enhancement of known IDC (arrowhead). Suspicious NME is not visualized. Given the absence of a CEM correlate to serve as biopsy target, CEM-guided biopsy was canceled. Subsequent MRI-guided biopsy of suspicious NME was completed; histologic assessment yielded IDC, deemed concordant by the performing radiologist. Image courtesy of the ARRS.
(A, B) Images depict a 65-year-old woman with prior left malignant lumpectomy. (A) Sagittal fat-suppressed contrast-enhanced T1-weighted image from diagnostic MRI performed for clear left nipple discharge shows segmental nonmass enhancement (NME) (arrows), deemed suspicious with assessment as BI-RADS category 4. The patient elected to undergo attempted contrast-enhanced mammography (CEM)-guided biopsy rather than direct MRI-guided biopsy. (B) Recombined scout image from attempted CEM-guided biopsy shows corresponding NME (arrows), serving as the biopsy target. CEM-guided biopsy was completed. Histologic assessment yielded benign findings, deemed concordant by the performing radiologist. (C,D) Images depict a 55-year-old woman with left breast invasive ductal carcinoma (IDC). (C) Sagittal fat-suppressed contrast-enhanced T1-weighted MR image from staging MRI shows known IDC (arrowhead) and additional 4-mm NME (arrow), deemed suspicious with assessment as BI-RADS category 4. Only NME was considered to represent a suspicious finding warranting biopsy. The patient elected to undergo attempted CEM-guided biopsy rather than direct MRI-guided biopsy. (D) Recombined scout image from attempted CEM-guided biopsy shows an enhancement of known IDC (arrowhead). Suspicious NME is not visualized. Given the absence of a CEM correlate to serve as biopsy target, CEM-guided biopsy was canceled. Subsequent MRI-guided biopsy of suspicious NME was completed; histologic assessment yielded IDC, deemed concordant by the performing radiologist. Image courtesy of the ARRS.
Six of the 21 women had a biopsy target identified by CEM and underwent CEM-guided biopsy; all of these were benign. The remaining 15 women lacked a CEM correlate to serve as a biopsy target and CEM-guided biopsy was canceled after CEM was continued for an average of 8.5 minutes.
These 15 women underwent MRI-guided biopsy. Of these, 13 completed the MRI-guided biopsy, which yielded the following findings: eight benign findings, two high-risk lesions, two invasive ductal carcinomas, and one ductal carcinoma in situ (DCIS). This yielded an overall malignancy rate of 27%.
The radiologists deemed all completed CEM-guided and MRI-guided biopsies concordant. After CEM-guided biopsy, three women underwent diagnostic mammography and one underwent CEM six months post-biopsy, all without suspicious findings.
The team also assessed target conspicuity in the six women who underwent completed CEM-guided biopsy and the 13 who underwent MRI-guided biopsy, using a 5-point Likert scale to measure conspicuity. Median target conspicuity for CEM and MRI for both readers was 1 and 3.
Finally, among the 15 women with canceled CEM-guided biopsy, both readers identified one CEM target corresponding to the suspicious MRI finding that was not recognized prospectively. MRI-guided biopsy deemed this lesion to be malignant.
Morris said the team will next explore two areas in CEM-guided biopsy: Determining whether increasing iodine load by increasing contrast volume will improve target conspicuity and exploring how changes to the CEM post-processing algorithm impact target conspicuity.
“Over time, the learning curve for operators [radiologists and technologists] may improve CEM-guided biopsy techniques and evolving post-processing algorithms may improve CEM target conspicuity,” Morris told AuntMinnie.com.
The full study can be accessed here.