A newly developed Musculoskeletal Infection-Reporting and Data Systems (MSKI-RADS) framework is effective when it comes to standardized terminology and recommended management of MRI findings of extremity infections, researchers have reported.
A team led by Avneesh Chhabra, MD, of the University of Texas Southwestern Medical Center in Dallas, found that the system's overall accuracy was higher than final diagnoses rendered without using it, at 65% compared with 55%. The study results were published August 27 in Radiology.
"The [MSKI-RADS] is a valid and reliable system for standardized terminology and recommended management of imaging findings of extremity infections across varying musculoskeletal fellowship-trained reader experience levels," the group wrote.
Incidence of osteomyelitis is climbing, due in part to increased prevalence of diabetes, cancer, and reduced overall immunity, Chhabra and colleagues wrote. It is treated with long-term antibiotic therapy and/or surgery -- both of which contribute to healthcare costs (for example, diabetic foot osteomyelitis costs Medicare up to $13 billion per year, they explained). X-ray imaging helps clinicians locate and confirm osteomyelitis and assess its scope; MRI with contrast is used to confirm x-ray results. But a consistent interpretation system for MRI results has been lacking.
To address this problem, Chhabra's group designed the MSKI-RADS system and assessed its efficacy using data from 208 adult patients with suspected extremity infections who underwent both x-ray and MRI exams between June 2015 and May 2019. The MSKI-RADS scoring system is as follows:
- 0, incomplete imaging
- I, negative for infection
- II, superficial soft-tissue infection
- III, deeper soft-tissue infection
- IV, possible osteomyelitis
- V, highly suggestive of osteomyelitis and/or septic arthritis
- VI, known osteomyelitis
- NOS (not otherwise specified), nonspecific bone lesions
The team calculated interreader agreement (using the intraclass correlation coefficient, or ICC) and true-positive rates of the MSKI-RADS system among 20 radiologists from 13 institutions with musculoskeletal radiology exam interpretation experience ranging from less than five years to more than 10 years.
The readers classified most of the paired x-ray/MRI exams as NOS, or "nonspecific bone lesions" (36, or 17%); followed by II, "superficial soft-tissue infection" (35, or 16.8%%); and V, "highly suggestive of osteomyelitis and/or septic arthritis" (also 35, or 16.8%). Interreader agreement for using the MSKI-RADS system among the 20 readers was moderate, with an ICC of 0.7, and the team found no correlation between reader experience and overall accuracy (p = 0.94).
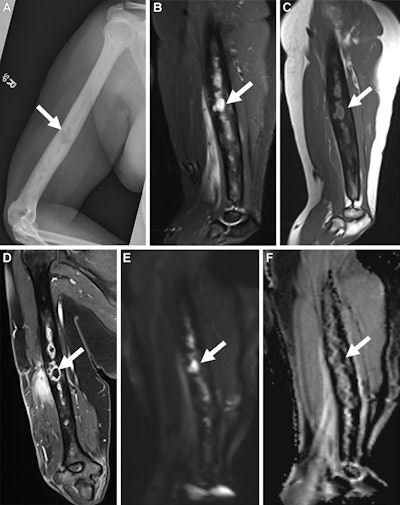 Musculoskeletal Infection Reporting and Data System (MSKI-RADS) category V findings in a 35-year-old female patient with infection in the right humerus. (A) Frontal radiograph, sagittal (B) short tau inversion recovery and (C) T1-weighted images, and (D) coronal Dixon fast spin-echo three-dimensional T1-weighted postcontrast image of the right humerus show osteomyelitis with intraosseous abscess (arrow), consistent with MSKI-RADS category Va, defined as highly suggestive of osteomyelitis. Corresponding (E) diffusion-weighted image and (F) apparent diffusion coefficient map show high signal intensity on E and low signal intensity on F, consistent with abscess (arrow). Image and caption courtesy of the RSNA.
Musculoskeletal Infection Reporting and Data System (MSKI-RADS) category V findings in a 35-year-old female patient with infection in the right humerus. (A) Frontal radiograph, sagittal (B) short tau inversion recovery and (C) T1-weighted images, and (D) coronal Dixon fast spin-echo three-dimensional T1-weighted postcontrast image of the right humerus show osteomyelitis with intraosseous abscess (arrow), consistent with MSKI-RADS category Va, defined as highly suggestive of osteomyelitis. Corresponding (E) diffusion-weighted image and (F) apparent diffusion coefficient map show high signal intensity on E and low signal intensity on F, consistent with abscess (arrow). Image and caption courtesy of the RSNA.
They also found that the highest true-positive rate was for MSKI-RADS I and NOS (both at 88.7%); the true-positive rate for MSKI-RADS V was 73%. Finally, Chhabra and colleagues noted that overall reader accuracy using MSKI-RADS across all patients was 65%, which was higher than final reader diagnoses without using the system (55%).
Using the MSKI-RADS system could improve patient care, according to the authors.
"By reducing confusion and minimizing usage of misleading terms, [the MSKI-RADS system] offers the potential to improve interdisciplinary communications across research facilities and patient care institutions," they concluded. "Its use can aid in efficient management decisions, improved patient outcomes, and better longitudinal collection of data for future research."
In an accompanying commentary, Mark Schweitzer, MD, of Wayne State University in Detroit, MI, called the MSKI-RADS system an "impressive springboard," noting that it "should not be held to the current LI-, PI-, or BI-RADS standards, which have the benefit of years of tweaking."
"[Similar] to malignancies, musculoskeletal infections are often biopsied," Schweitzer wrote. "If these infections are misclassified and then mistreated, the prognosis is poor. Thus, I believe that MSKI-RADS, in attempting to quantitate diagnosis and confidence, and relatedly the work-up (and treatment) recommendation, is an ambitious and notable first step."
The complete study can be found here.




















