SINGAPORE -- The use of MRI for musculoskeletal (MSK) trauma imaging is becoming increasingly viable, according to a presentation delivered May 7 at the International Society of Magnetic Resonance in Imaging (ISMRM) meeting.
"MRI is underutilized in trauma imaging and often falls short of its potential," said presenter Prof. Benjamin Fritz, MD, of Balgrist University Hospital in Zurich, Switzerland. Fritz moderated a session titled "Seeing the Unseen: MRI in Traumatic Musculoskeletal Disease."
X-ray and CT imaging are the go-to exams for trauma, Fritz conceded, but MRI is gaining ground as an effective modality for MSK trauma applications, in part because it does not expose patients to radiation and because it can image soft tissue well. There are obstacles to its use -- namely cost, more limited operating hours, a lack of available MRI technicians, and long acquisition/result turnaround times -- but MRI does have a place in the trauma imaging sphere.
Fritz outlined ways MRI can be made a viable trauma imaging option:
- Use of AI image reconstruction speed MRI exams.
- Use of fast imaging protocols (for example, four sequences that include sagittal T2, sagittal T1, sagittal Short Tau Inversion Recovery (STIR), and axial T2) can allow for an 11-minute exam from the time the patient enters the MRI to when the patient exits.
- Reducing result turnaround time by toggling two patients (use separate preparation rooms, an MRI suite with two doors, two docking tables and sets of coils, and two technologists). "This optimized MRI workflow resulted in a mean time savings of 5 minutes 28 seconds per patient," Fritz said.
He also described the benefits of ultrashort echo-time (UTE) MRI exams, which can image bone pathologies comparably to CT; Dixon imaging; and metal suppression techniques for imaging patients with implants (STIR, STIR with optimized inversion RF pulse [STIR WARP], and STIR Compressed Sensing [CS] slice encoding for metal artifact correction [SEMAC]).
 Sagittal view of the scapula showing a comminuted fracture of the inferior portion, imaged with computed tomography (CT, left image) and by an ultrashort time of echo (UTE) sequence (right image) on MRI. Both images appear similar, with an identical representation of the fracture, illustrating the potential of UTE to create CT-like images and suggesting that both imaging modalities could be interchangeable in clinical practice. All images and captions courtesy of Prof. Benjamin Fritz, MD.
Sagittal view of the scapula showing a comminuted fracture of the inferior portion, imaged with computed tomography (CT, left image) and by an ultrashort time of echo (UTE) sequence (right image) on MRI. Both images appear similar, with an identical representation of the fracture, illustrating the potential of UTE to create CT-like images and suggesting that both imaging modalities could be interchangeable in clinical practice. All images and captions courtesy of Prof. Benjamin Fritz, MD.
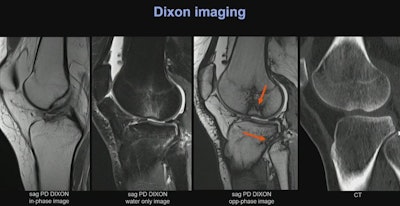 A 15-year-old female soccer player presented with a knee distortion featuring a pivot-shift injury mechanism and an osseous avulsion of the anterior cruciate ligament (left image). PD-weighted MRI images were acquired using the Dixon technique, capable of displaying bone marrow edema patterns at the lateral femoral condyle adjacent to a small cortical impression fracture, and at the proximal tibiofibular joint, indicative of a nondisplaced trabecular microfracture. In the opposed-phase images of the PD-weighted Dixon sequence, a typical linear hypointense artifact (India ink artifact) is visible along the borders of the trabecular microfractures, which can be beneficial in clinical practice for the detection of fractures. For comparison, a computed tomography image is provided on the right.
A 15-year-old female soccer player presented with a knee distortion featuring a pivot-shift injury mechanism and an osseous avulsion of the anterior cruciate ligament (left image). PD-weighted MRI images were acquired using the Dixon technique, capable of displaying bone marrow edema patterns at the lateral femoral condyle adjacent to a small cortical impression fracture, and at the proximal tibiofibular joint, indicative of a nondisplaced trabecular microfracture. In the opposed-phase images of the PD-weighted Dixon sequence, a typical linear hypointense artifact (India ink artifact) is visible along the borders of the trabecular microfractures, which can be beneficial in clinical practice for the detection of fractures. For comparison, a computed tomography image is provided on the right.
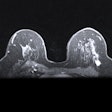
 Coronal STIR images of a total knee arthroplasty were acquired using clinical standard technique (left image) without metal suppression, high-bandwidth WARP technique (middle image), and compressed sensing (CS) SEMAC technique (right image). These images demonstrate decreasing metal artifacts from left to right and illustrate the applicability of these metal artifact suppression techniques in clinical practice.
Coronal STIR images of a total knee arthroplasty were acquired using clinical standard technique (left image) without metal suppression, high-bandwidth WARP technique (middle image), and compressed sensing (CS) SEMAC technique (right image). These images demonstrate decreasing metal artifacts from left to right and illustrate the applicability of these metal artifact suppression techniques in clinical practice.
So where is radiology heading when it comes to using MRI for musculoskeletal trauma? Definitely toward increased use, according to Fritz.
"We're heading towards higher accessibility of MRI in emergency settings, faster MR imaging, improved bone visualization on MRI, and improved metal imaging," he concluded. "This will result in higher employment of MRI in trauma patients and in emergency radiology."