MRI performed after treatment of locally advanced rectal cancer can offer value in predicting patient outcomes, according to research published September 3 in Radiology.
“Restaging MRI can stratify patients treated with total neoadjuvant therapy into clinical response categories predictive of organ preservation, local regrowth, and survival,” wrote a multi-institutional research team led by first author Hannah Williams, MD, and senior author Julio Garcia-Aguilar, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York City.
Although MRI has long played a crucial role in restaging locally advanced rectal cancer that’s been treated with total neoadjuvant therapy, there haven’t been any prospective studies that have evaluated the modality’s capability to accurately select patients for nonoperative management, according to the researchers.
In an effort to assess MRI’s restaging performance in predicting oncology outcomes and to identify imaging features associated with residual disease after total neoadjuvant therapy, the authors performed a secondary analysis of the Organ Preservation in Rectal Adenocarcinoma (OPRA) trial.
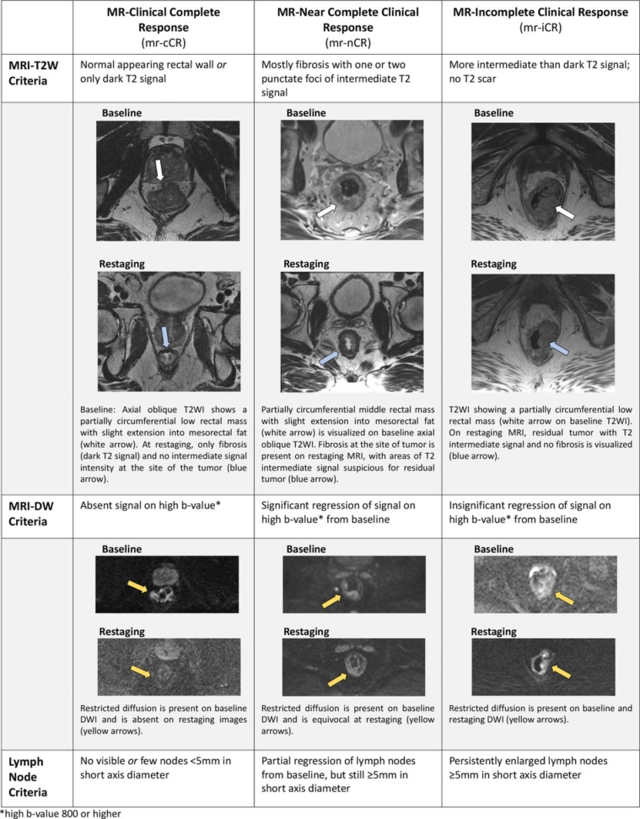 Chart shows the T2-weighted imaging (T2W, T2WI), diffusion-weighed imaging (DW, DWI), and lymph node criteria used to categorize MRI-based response as clinical complete response (mr-cCR), near-complete clinical response (mr-nCR), or incomplete clinical response (mr-iCR). * = b ≥ 800 sec/mm². Images and caption courtesy of the RSNA.
Chart shows the T2-weighted imaging (T2W, T2WI), diffusion-weighed imaging (DW, DWI), and lymph node criteria used to categorize MRI-based response as clinical complete response (mr-cCR), near-complete clinical response (mr-nCR), or incomplete clinical response (mr-iCR). * = b ≥ 800 sec/mm². Images and caption courtesy of the RSNA.
Conducted between April 14 and March 2023, OPRA randomized patients with stages II or III rectal adenocarcinoma to undergo either induction or consolidation total neoadjuvant therapy. In their current study, the researchers specifically analyzed the results of patients who had undergone restaging MRI.
Radiologists assessed restaging MRI exams performed a mean of eight weeks after treatment for 277 patients as having a clinical complete response, near-complete clinical response, or incomplete clinical response.
| Disease-free survival rate by MRI response category | |||
|---|---|---|---|
| Incomplete clinical response | Near-complete clinical response | Clinical complete response | |
| Five-year disease free survival | 49.6% | 67.6% | 81.8% |
In other results, the MRI response category also predicted overall survival (p < 0.001), distant recurrence-free survival (p = 0.005), and local regrowth (p = 0.02). After performing multivariable analysis, the authors also found that the presence of restricted diffusion (odds ratio = 2.5, with 1 as reference) and abnormal nodal morphologic features (odds ratio = 5.04) were independently associated with residual disease.
“Future research should focus on integrating findings from both posttreatment endoscopy and MRI, as the combined result better reflects clinical practice and likely provides greater prognostic value than individual assessment,” they wrote.
In an accompanying editorial, Laurent Milot, MD, PhD, of the University of Lyon in France noted that the study will motivate further research.
“Despite some limitations inherent to MRI itself, by providing an MRI classification of response to treatment that is linked to clinically relevant outcomes, the study by Williams and Omer et al shines a light regarding the potential role of MRI in the emerging and fast-developing area of watch-and-wait management for organ preservation in patients with rectal cancer,” he wrote.
The full article and accompanying editorial can be found here and here.