Simulated contrast-enhanced MR images from noncontrast sequences using deep learning show promise for assessing clinically significant prostate cancer, according to a study published January 14 in Radiology.
The findings could mitigate patients' exposure to contrast, wrote a team led by Hongyan Huang, MD, of Shenzhen University in China.
"In [our] study, we … demonstrated the feasibility of simulating contrast-enhanced images from noncontrast prostate MRI sequences," the group noted. "These findings could potentially reduce the necessity of gadolinium-based contrast agent administration."
Multiparametric MRI -- including contrast-enhanced sequences -- is recommended for evaluating suspected prostate cancer, the group explained. But some have raised concerns about potential contrast agent accumulation (specifically, gadolinium) and toxicity, it wrote, noting that "contrast-enhanced imaging requires intravenous injection of a gadolinium-based contrast agent and physician monitoring, which decreases patient throughput and increases health care costs," and that "gadolinium-based contrast agents can trigger allergic reactions and potentially cause toxicity and accumulation in the body."
That's why it's important to find a way to achieve the same effect without contrast, according to Huang and colleagues. To this end, they explored whether using deep learning with non-contrast MRI sequences could produce simulated contrast-enhanced MR images that could help clinicians assess clinically significant prostate cancer using PI-RADS version 2.1. Their research included 567 men with suspected prostate cancer who underwent multiparametric MRI between April 2020 and April 2023.
The team trained a deep-learning model (i.e., a pix2pix algorithm) to synthesize contrast-enhanced MRI scans from four noncontrast MRI sequences (T1-weighted imaging, T2-weighted imaging, diffusion-weighted imaging, and apparent diffusion coefficient maps), then tested the model on an internal (104 exams) and two external datasets (test set one, 143 exams and test set two, 76 exams). Three radiologists independently scored T2-weighted and diffusion-weighted MR images with either simulated or acquired contrast-enhanced images using PI-RADS 2.1, and the investigators assessed agreement between these interpretations with the Cohen's kappa coefficient.
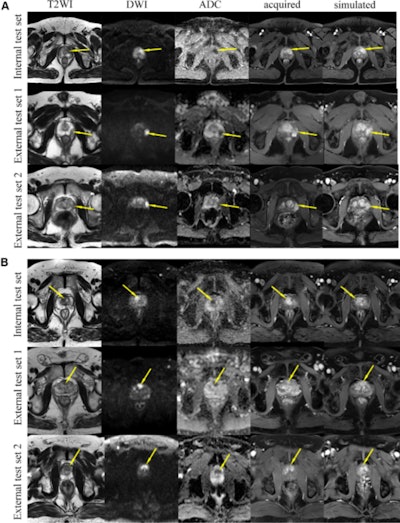 Axial prostate MRI scans. The simulated contrast-enhanced axial prostate images were comparable with the acquired contrast-enhanced images. Example images from the internal test set and the two external test sets show (A) a lesion in the peripheral zone (arrows) and (B) a lesion in the transition zone (arrows). Notably, there are visual differences between the simulated and acquired contrast-enhanced images regarding the degree of lesion enhancement and the measurement of lesion size (see Fig S4). ADC = apparent diffusion coefficient, DWI = diffusion-weighted imaging, T2WI = T2-weighted imaging. Images and caption courtesy of the RSNA.
Axial prostate MRI scans. The simulated contrast-enhanced axial prostate images were comparable with the acquired contrast-enhanced images. Example images from the internal test set and the two external test sets show (A) a lesion in the peripheral zone (arrows) and (B) a lesion in the transition zone (arrows). Notably, there are visual differences between the simulated and acquired contrast-enhanced images regarding the degree of lesion enhancement and the measurement of lesion size (see Fig S4). ADC = apparent diffusion coefficient, DWI = diffusion-weighted imaging, T2WI = T2-weighted imaging. Images and caption courtesy of the RSNA.
Huang's group found that the simulated and acquired contrast-enhanced images were comparable as calculated by the multiscale structural similarity index (which measures the quality of images and videos, with 1 as reference), showing values of 0.82 for the internal test set, 0.71 for external test set one, and 0.69 for external test set two.
Finally, the team reported that when they added simulated contrast-enhanced imaging to biparametric MRI, 34 of 323 (10.5%) patients were upgraded from PI-RADS 3 to PI-RADS 4.
The study "highlights the potential of generative AI in synthesizing contrast-enhanced prostate MRI," wrote Radhouene Neji, MD, and colleague Vicky Goh, MD, both of King's College London in the U.K., in an accompanying commentary.
"Ongoing progress in generative AI for prostate MRI requires that large multicentric benchmark datasets be brought together," Neji and Goh wrote. "It also requires challenges to be organized by the radiology, computer vision, and image processing AI communities to compare the performance and robustness of different generative AI models for the synthesis of contrast-enhanced data such as the one proposed in this study. Finally, future prospective multicenter studies are necessary to confirm the clinical value of generative AI. We look forward to that."
The complete study can be found here.