Are low-field MRI units effective for neuroradiologic imaging? Perhaps, say researchers from the University of Michigan in Ann Arbor -- but more technological development is needed.
Use of low-field MRI for this indication would improve patient care by expanding access to the modality, wrote a team led by medical student Lauren Kelsey. The group's commentary was published February 13 in RadioGraphics.
"MRI for diagnosis and assessment of neurologic conditions is most commonly performed on 1.5-tesla and 3-tesla systems," Kelsey and colleagues noted. "[But] recently, motivation to increase accessibility to MRI, coupled with advances in software and hardware, has sparked renewed interest in MRI systems with magnetic field strengths ranging from 0.064-tesla to 1-tesla."
It's true that overall image quality of routine clinical brain and spinal MR imaging at 0.55-tesla is lower than that at 1.5-tesla, but low-field MRI remains diagnostic for many indications, the authors explained, and the "intrinsic benefits of using a lower main magnetic field strength may be leveraged for imaging intracranial and spinal hardware due to diminished susceptibility artifacts and pose new opportunities for increased MRI safety." Also, using low-field MRI may make imaging of structures near bone -- such as the internal auditory canal -- more feasible, they wrote.
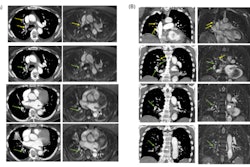
 Acute right middle cerebral artery territory infarction (arrows) in a 66-year-old man, imaged at 1.5-tesla first and then at 0.55-tesla nine days later. Initial 1.5-tesla MRI images (top row) show diffusion restriction with associated mild T2 prolongation, compatible with acute infarction. On the subsequent 0.55-tesla images (bottom row), there is expected evolution of the infarct, with normalization of the apparent diffusion coefficient (ADC) map. Acquisition times for FLAIR imaging were 2 minutes, 45 seconds (with deep learning reconstruction) for 1.5-tesla imaging and 4 minutes, 14 seconds for 0.55-tesla imaging. The acquisition times for DWI were 1 minute, 3 seconds for 1.5-tesla imaging and 2 minutes, 52 seconds for 0.55-tesla imaging. Images and caption courtesy of the RSNA.
Acute right middle cerebral artery territory infarction (arrows) in a 66-year-old man, imaged at 1.5-tesla first and then at 0.55-tesla nine days later. Initial 1.5-tesla MRI images (top row) show diffusion restriction with associated mild T2 prolongation, compatible with acute infarction. On the subsequent 0.55-tesla images (bottom row), there is expected evolution of the infarct, with normalization of the apparent diffusion coefficient (ADC) map. Acquisition times for FLAIR imaging were 2 minutes, 45 seconds (with deep learning reconstruction) for 1.5-tesla imaging and 4 minutes, 14 seconds for 0.55-tesla imaging. The acquisition times for DWI were 1 minute, 3 seconds for 1.5-tesla imaging and 2 minutes, 52 seconds for 0.55-tesla imaging. Images and caption courtesy of the RSNA.
The investigators acknowledged that lower-field MRI systems carry some challenges, including acceleration artifacts and insufficient signal intensity of dynamic contrast-enhanced susceptibility-weighted perfusion imaging -- which can impede evaluation of multiple sclerosis and primary brain tumors.
What's needed, Kelsey and colleagues wrote, is further exploration of applications of 0.55-tesla MRI that are particularly advantageous at lower field strengths, such as those in "balanced steady-state free-precession and single-shot fast spin-echo MRI, which are being used in functional and fetal MRI."
Another strategy to make low-field MRI more effective is using deep learning to improve image quality on low-field MRI while also maintaining or reducing exam times; the group referred to previous research on the use of AI with low-field MRI that showed reduced acquisition times for axial (24%) and sagittal (23%) cervical images, axial (41%) and sagittal (33%) thoracic images, and sagittal lumbar (36%) images.
Use of "midfield" MRI systems (i.e., 0.35-tesla to 1-tesla) could free up systems with higher field strengths, the group noted.
"Modern midfield systems have the potential to improve access to MRI as they require fewer resources to acquire and maintain," the team wrote. "For institutions that have MRI systems at other field strengths (typically 1.5-tesla or 3-tesla), identifying entities that may be adequately imaged at 0.55-tesla may also help improve efficiency, as the higher–field-strength units may then be reserved for conditions where it is an absolute requirement."
Although midfield MRI systems show promise for diagnostic imaging, they will require more software and hardware development, wrote Vivek Pai, MD, and Pejman Jabehdar Maralani, MD, both of University of Toronto in Canada, in an accompanying commentary.
"Advantages to using midfield MRI systems such as lenient siting requirements, reduced acquisition costs, and potentially better safety profiles in patients with implanted devices can improve MRI accessibility and health care equity," the two wrote. "However, there are several drawbacks that need to be addressed and accounted for. Despite deep learning-related solutions, improvements in signal-to-noise ratio and imaging times need to be further interrogated, given that these systems have immense potential for imaging in critical and emergent cases."
The complete study can be found here.