An emerging MRI brain biomarker called free water fraction is increased in patients with Alzheimer's disease compared with their healthy counterparts, according to a study published October 7 in Radiology.
The finding is from a secondary analysis of 359 participants from a previous Alzheimer’s disease study. This analysis further found that free water fraction was associated with beta amyloid and tau, two hallmark brain PET imaging biomarkers, noted lead author Junfang Zhang, PhD, of Shanghai Jiao Tong University in Shanghai, China, and colleagues.
“These findings highlight the role of free water in juxtacortical [white matter] as a major contributor to [Alzheimer's disease] pathogenesis, providing new insights that complement our understanding of amyloid deposition,” the group wrote.
In Alzheimer’s disease, cellular atrophy decreases brain tissue, reduces water bound to neurites, and increases free water. That's why free water fraction (FWF) measured using diffusion MRI is an emerging and sensitive microstructural marker that could help detect early atrophy in the brain, the researchers explained.
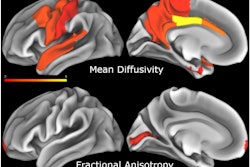
To date, spatiotemporal changes of FWF in juxtacortical white matter -- the layer that lies immediately adjacent to the brain’s outer layer of gray matter -- have not been studied in Alzheimer’s disease, the group noted. In this study, the researchers evaluated juxtacortical FWF, its association with neuropathologic disease severity, and its spatiotemporal pattern using MRI and PET in participants with Alzheimer’s disease or normal cognition.
The group gathered data from 359 participants from a previous trial who had undergone diffusion MRI, F-18 florbetapir PET to assess beta amyloid deposits, and F-18 MK-6240 PET to assess tau accumulation. The group included control participants with normal cognition (n = 161), patients with mild cognitive impairment due to Alzheimer’s disease (n = 85), and patients with dementia due to Alzheimer’s (n = 113).
According to the analysis, compared with controls, participants with Alzheimer’s disease had increased FWF, which was associated with higher global cortical beta amyloid and tau deposits, the researchers reported.
 A graphical abstract.RSNA
A graphical abstract.RSNA
In addition, using two machine-learning models for identifying subgroups, the researchers found distinct patterns of FWF alteration. In the first model, participants with an orbitofrontal-first subtype had smaller hippocampus volumes (left, p = 0.007; right, p = 0.03) and worse cognitive performance (verbal fluency test, p = 0.01; shape-trail test part A, p < 0.001). In the second model, they identified unique FWF and beta amyloid progression patterns, each of which showed variations in neurodegeneration and cognitive function profiles.
“Juxtacortical free water fraction, determined at diffusion MRI, was higher in participants with Alzheimer's disease compared with cognitively normal controls and associated with [beta amyloid], tau, and neurodegeneration biomarkers, revealing two distinct spatiotemporal progression patterns with different impacts on neuroanatomic signatures and cognitive performance,” the group wrote.
Future longitudinal studies with larger sample sizes are needed to offer further insights into the relationships between these FWF subtypes and Alzheimer’s disease pathology, the authors concluded.
In an accompanying editorial, Menno Schoonheim, PhD, of Amsterdam UMC in the Netherlands, wrote that the results underscore that white-matter damage in juxtacortical areas is common and can occur early in Alzheimer’s disease, yet the type of damage detected is subtle and remains difficult to quantify.
“Implementation [of measuring free water fraction] would require clear cutoff scores of abnormal diffusion across patient populations and scanner types," Schoonheim wrote. "[It] would also require expanding MRI protocols with more frequent scans, which is always a challenge."
Despite these potential difficulties, the findings outline an important step toward better understanding of the relevance and staging of white-matter pathologic abnormalities in patients with Alzheimer’s disease, he concluded.
The full study is available here.