The inability of physicians to recognize radiation-induced changes in the skin can lead to misdiagnoses and incorrect treatment, according to a review in the July American Journal of Roentgenology.
In a two-part series, Dr. Titus Koenig from the University of Texas Medical School in Houston and his co-authors summarized the most common skin injuries from fluoroscopically guided procedures. They also made recommendations for minimizing radiation dose delivery.
"The incidence of radiation injuries is small compared with the number of procedures performed. More than 700,000 interventional cardiologic and other procedures are now performed each year. Dermatologists and interventionalists must be aware of the potential for skin injuries and recognize the characteristics of such injuries," wrote the authors (AJR, July 2001, Vol.177:1, pp. 1-20). In addition to Koenig, the researchers hailed from the University of New Mexico School of Medicine in Albuquerque and the Moerser Landstr. 352 in Krefield, Germany
Part 1 of the series details the characteristics of radiation injury, including radiodermatitis, sublethal cell injuries, and desquamation of the skin. Threshold doses and the types of responses to look for after irradiation are outlined.
One section addresses the criteria for radiation sensitivity. Previous investigators have reported that the degree of skin response to radiation varies for different body sites, the authors said. In addition, patients generally do not return to the doctor who performed the radiation therapy for a skin problem.
"Usually they present at some stage to a dermatologist, but do not give a history of prior fluoroscopy because they assume it is irrelevant for the complaint or have forgotten about it," the authors said.
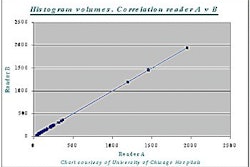
In Part 2, the authors review 73 cases and offer suggestions for lowering dose delivery to patients. In the case of 47 patients who underwent coronary angiography, the reviewers found significantly longer fluoroscopic times, as long as 172 minutes for a single procedure, in patients with skin injuries.
"All patients had skin damage," they wrote. "After a prolonged erythema, a nonhealing skin ulceration developed in the region of the right scapula, possibly as a result of biopsy. The lesion required skin grafting."
Some of the technical factors that can reduce skin damage include cutting down on exposure times to the same skin area and using a scatter-removing pad. They also recommend the installation of real-time dose-monitoring equipment.
"Dose is a far more relevant indicator of risk than fluoroscopy on-time, and monitoring it eliminates the need to monitor fluoroscopy time. Knowing the skin dose, or at least the approximation of it, will assist physicians in the benefit-risk decisions concerning potential alternative actions when dose accumulation becomes a concern," they said.
In an accompanying commentary, Dr. Lee Rogers, AJR editor-in-chief, decried the use of fluoroscopy by other disciplines who are "left to their own devices. It is wrong to be allowed to obtain credentials at weekend courses. Paying lip service to the requirements for knowledge of radiation is to be deplored."
By Shalmali PalAuntMinnie.com staff writer
June 21, 2001
Related Reading
Eight reported dead in Panama after radiation therapy, June 6, 2001
FDA's radiation concerns may lead to dose displays for scanners, May 22, 2001
FDA worried about radiation risk from whole-body CT for routine screening, May 18, 2001
Burn cream reduces skin toxicity during radiation therapy for breast cancer, September 23, 2000
Click here to post your comments about this story. Please include the headline of the article in your message.Copyright © 2001 AuntMinnie.com